Oncology
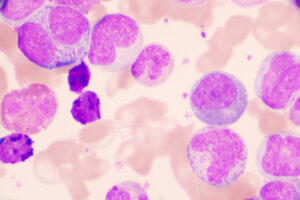
Chronic Lymphocytic Leukemia
Initiating Novel Agents Versus Chemoimmunotherapy in the Front-line Setting
Overview
With the introduction of novel therapies for chronic lymphocytic leukemia (CLL), interest in the possibility of earlier treatment has led to the initiation of several ongoing clinical trials. In this roundtable discussion, experts in the field Jennifer R. Brown, MD, PhD, Jan A. Burger, MD, PhD, and Anthony Mato, MD, MSCE, note the absence of current data to support this practice and discuss why earlier treatment is not necessarily better in managing patients with CLL. They also offer their perspectives on chemoimmunotherapy versus novel therapies in the front-line setting.
Q: In your clinical judgment, when should therapy be initiated for patients diagnosed with CLL?
Jan A. Burger, MD, PhD
|
|
|
Regarding when to initiate therapy for CLL, I think that perhaps some of this is coming from the notion that the novel agents, in general, are perceived as less toxic and therefore the question is, “Why should we not treat patients earlier with agents that are so well tolerated?” However, in my opinion, we should not always recommend early treatment for the same reasons that we have not recommended chemoimmunotherapy as treatment for early stage or asymptomatic CLL. I think that the consensus is still clear that patients who are asymptomatic or have early stage CLL should not be treated. Studies are investigating the question of treating earlier, but I am skeptical about this approach because there is always a risk of overtreating patients. If they are asymptomatic, you may get improvements in numbers, but not necessarily in patient well-being, and even the new agents have the potential for significant side effects. We also should not forget that, in some patients, CLL behaves as a very indolent disease. Approximately 30% of patients have CLL that is so indolent that they will not progress to a point where they need treatment throughout their lifetime. So, there are a substantial number of asymptomatic patients who we would overtreat by pushing for early treatment. Collectively, the reasons for not moving treatment to patients with early stage disease who have no symptoms are multiple: no data, potential for overtreatment, costs, and potential side effects. |
|
Anthony R. Mato, MD, MSCE
|
|
“Amongst practitioners, I think that there may be some excitement to potentially begin novel agents earlier. I think that that is, in part, because of the activity of these agents and the fact that they are relatively easy to give.”
Amongst practitioners, I think that there may be some excitement to potentially begin novel agents earlier. I think that that is, in part, because of the activity of these agents and the fact that they are relatively easy to give. Toward that enthusiasm, I would also argue caution; there is no study to suggest that intervening early for any patient population with any modern therapy can improve outcomes. And so, I think that the International Workshop on Chronic Lymphocytic Leukemia (iwCLL) recommendations for when to initiate therapy are the most appropriate and are the standard of care.
Jennifer R. Brown, MD, PhD
|
|
|
I agree completely, and I would definitely also urge caution about initiating therapy only when therapy is truly indicated by the iwCLL criteria. Most of the data that we have for adverse clonal evolution of the disease occur in the setting of therapy. And so, avoiding therapy until we have clear evidence that earlier therapy is helpful is most prudent. |
|
Q: In the font-line setting, how do you generally approach the selection of chemoimmunotherapy versus novel agents for patients with CLL?
Jan A. Burger, MD, PhD
|
|
“To synopsize, comorbidity and age have been strong influential factors for the selection of chemoimmunotherapy; nonetheless, these treatments are used less often now with the emergence of the novel agents.”
The decision is guided by numerous clinical, prognostic, and patient-specific factors, which we discuss at length when considering the implications of age and fitness. However, to synopsize, comorbidity and age have been strong influential factors for the selection of chemoimmunotherapy (where either an intensive backbone with fludarabine/cyclophosphamide, or a less intensive backbone with bendamustine, or an even less intensive backbone with chlorambucil is used). Nonetheless, these treatments are used less often now with the emergence of the novel agents. We currently use the immunoglobulin heavy chain variable region (IGHV ) gene mutational status as a stratifying factor to determine whether patients would be candidates for chemoimmunotherapy. If they are mutated, we have long-term experience with fludarabine, cyclophosphamide, and rituximab (FCR), and we know that approximately 60% of patients remain in remission beyond 10 years if they have the lower-risk feature of mutated CLL. And for those patients, we still offer the FCR program, although, currently, we make efforts to reduce the number of administered chemoimmunotherapy cycles. Then, the cytogenetic markers are also helpful with assessing the risk of eventually relapsing after chemoimmunotherapy or on novel agents.
It is probably best to go one-by-one: 17p deletion (del[17p]) status is very important to know at the time when you have to make a choice about treatment because you do not want to use chemoimmunotherapy for any patient who has del(17p). If you put such patients on treatment with novel agents, those are patients who, in the front-line setting, but especially in the relapse setting, have higher risk of progressing, and one should be aware of that in order to have discussions about cellular therapy such as allogeneic hematopoietic stem cell transplantation or chimeric antigen receptor T-cell therapy. Another factor detected with the CLL fluorescence in situ hybridization cytogenetic panel is del(11q); patients with del(11q) are often younger male patients who are IGHV unmutated, and such individuals have shorter than average remission durations with chemoimmunotherapy, hence this, again, favors the use of novel agents over chemoimmunotherapy.
We recently published long-term findings in a population of both treatment-naïve and relapsed/refractory patients who received ibrutinib, which is the most commonly used novel agent for CLL, in Blood. Data on the efficacy and safety of ibrutinib were analyzed with a median follow-up of 5 years in 31 treatment-naïve patients and 101 patients with relapsed/refractory CLL/small lymphocytic lymphoma. Our 5-year experience with single-agent ibrutinib in patients with treatment-naïve and relapsed/refractory CLL showed that efficacy of long-term treatment with ibrutinib was sustained despite the presence of high-risk genomic features in a large proportion of our patient population.
Anthony R. Mato, MD, MSCE
|
|
“First and foremost is determining whether there is P53 interruption or del(17p), and also whether there are 3 or more abnormalities in the karyotype (ie, complex karyotype)—and then also the IGHV mutational status—and these things are probably the biggest drivers for prognosis with the novel agents and with the chemoimmunotherapy combinations.”
First and foremost is determining whether there is P53 interruption or del(17p), and also whether there are 3 or more abnormalities in the karyotype (ie, complex karyotype)—and then also the IGHV mutational status—and these things are probably the biggest drivers for prognosis with the novel agents and with the chemoimmunotherapy combinations.
Jennifer R. Brown, MD, PhD
|
|
“Our highest-risk patients continue to be those with del(17p) or TP53 mutation, and this is true probably even with any of our newer therapies. Thus, it is important to identify these patients up front, for triage away from chemoimmunotherapy and toward novel agent therapies.”
Our highest-risk patients continue to be those with del(17p) or TP53 mutation, and this is true probably even with any of our newer therapies. Thus, it is important to identify these patients up front, for triage away from chemoimmunotherapy and toward novel agent therapies. Other important factors continue to include the IGHV mutation status and certain patient-specific factors (eg, age, comorbidities, stage of disease). Stage is less important than it used to be, but it is still significant.
References
Byrd JC, Furman RR, Coutre SE, et al. Three-year follow-up of treatment-naïve and previously treated patients with CLL and SLL receiving single-agent ibrutinib. Blood. 2015;125(16):2497-2506.
Hallek M, Cheson BD, Catovsky D, et al. Guidelines for diagnosis, indications for treatment, response assessment and supportive management of chronic lymphocytic leukemia. Blood. 2018 Mar 14. pii: blood-2017-09-806398. doi: 10.1182/blood-2017-09-806398. [Epub ahead of print]
Hallek M, Shanafelt TD, Eichhorst B. Chronic lymphocytic leukaemia. Lancet. 2018;391(10129):1524-1537.
Itchaki G, Brown JR. Experience with ibrutinib for first-line use in patients with chronic lymphocytic leukemia. Ther Adv Hematol. 2018;9(1):3-19.
Kipps TJ. Outcomes of ibrutinib-treated patients with chronic lymphocytic leukemia/small lymphocytic leukemia with high-risk prognostic factors in an integrated analysis of 3 randomized phase 3 studies. XVII International Workshop on Chronic Lymphocytic Leukemia; May 12-15, 2017; New York, NY.
Nabhan C, Raca G, Wang YL. Predicting prognosis in chronic lymphocytic leukemia in the contemporary era. JAMA Oncol. 2015;1(7):965-974.
O’Brien S, Furman RR, Coutre S, et al. Single-agent ibrutinib in treatment-naïve and relapsed/refractory chronic lymphocytic leukemia: a 5-year experience. Blood. 2018;131(17):1910-1919.
U.S. National Library of Medicine. ClinicalTrials.gov. A pilot study of a personalized neoantigen cancer vaccine with and without low-dose cyclophosphamide in treatment naïve, asymptomatic patients with IGHV unmutated chronic lymphocytic leukemia. https://clinicaltrials.gov/ct2/show/NCT03219450. Accessed May 24, 2018.