Oncology
Gastroenteropancreatic Neuroendocrine Tumors
Gastric Neuroendocrine Tumors: Updates and Perspectives
Gastric neuroendocrine tumors (G-NETs) have traditionally been classified into 3 types; however, some cases do not fit into the current classification categories, such as those associated with long-term proton pump inhibitor (PPI) use. Researchers at the 2024 ASCO Gastrointestinal Cancers Symposium presented data from a study characterizing PPI-associated G-NETs and comparing them with the existing G-NET classification types.
Following this presentation, featured expert Jonathan R. Strosberg, MD, was interviewed by Conference Reporter Editor-in-Chief Tom Iarocci, MD. Dr Strosberg’s clinical perspectives on these findings are presented here.
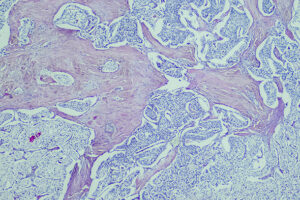
G-NETs are a poorly understood subset of NETs that are increasing significantly in incidence. Traditionally, we have classified G-NETs into 3 types. Type 1 is the most common and is associated with underlying chronic atrophic gastritis. Basically, the parietal cells of the stomach stop producing acid because of autoimmune disease. The resulting gastrin that is produced by the antrum of the stomach leads to the proliferation of enterochromaffin-like (neuroendocrine) cells in the stomach, and, over time, these can form small tumors, usually polyps. Type 1 G-NETs are small and benign in most cases. There are some exceptions, but if they are smaller than 1 to 2 cm in diameter, they tend to be low grade and almost never metastasize. And even metastatic type 1 G-NETs tend to be very indolent. Overall, this is usually a benign disease, so the standard recommendation is endoscopy and polypectomy every 1 to 2 years.
Type 2 is very rare and is associated with underlying gastrinoma, often in the setting of multiple endocrine neoplasia that cause NETs to form in the stomach. The treatment for this type of G-NET involves managing the underlying gastrinoma.
Type 3 G-NETs are sporadic in nature, meaning that there is no underlying atrophic gastritis or gastrinoma; these tumors arise on their own. They tend to be more malignant and are often managed with formal resection, just as you would do for an adenocarcinoma. However, if they are small and relatively low grade, you can try to manage type 3 G-NETs endoscopically.
While G-NETs are traditionally classified into those 3 types, another type of G-NET that we are increasingly seeing appears to be associated with chronic PPI use. PPIs can cause hypergastrinemia, similar to what occurs in patients with types 1 and 2 G-NETs, so we are unsurprisingly starting to see evidence that G-NETs may arise through this mechanism. This type of G-NET probably takes quite a few years to develop, so it is more likely to be found in patients who have been taking PPIs for 5 or 10 years, or even longer. In most cases, it is an incidental finding, so the more esophagogastroduodenoscopies people undergo, the more we will see it.
PPI-associated G-NETs seem to be less aggressive than completely sporadic tumors because the associated rate of distant metastases is quite low. That has been published in several small series in the last 5 years. We presented an even larger series at the North American Neuroendocrine Tumor Society (NANETS) 2023 Multidisciplinary NET Medical Symposium, where we saw very few distant metastases in patients who had been on chronic PPI therapy. And at the 2024 ASCO Gastrointestinal Cancers Symposium, data were presented from The University of Texas MD Anderson Cancer Center showing that only approximately 10% of patients with PPI-associated G-NETS presented with distant metastases (abstract 597).
I think that we need to figure out how many years of PPI therapy are required for a G-NET to be considered PPI associated. Of course, a lot of patients take PPIs, and they may develop truly sporadic tumors, but I have little doubt that PPI-associated G-NETs are a real entity. They need to be considered so that we do not overtreat these patients, as we do not recommend radical surgery for tumors with a low risk of metastases. So, I think that it would be appropriate for G-NETs to be reclassified with the addition of a new category of PPI-associated tumors.
Al-Toubah T, Pelle E, Strosberg J. Association of long-term PPI use with low-risk gastric neuroendocrine tumor [abstract C-55]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
Exarchou K, Howes N, Pritchard DM. Systematic review: management of localised low-grade upper gastrointestinal neuroendocrine tumours. Aliment Pharmacol Ther. 2020;51(12):1247-1267. doi:10.1111/apt.15765
Hu P, Bai J, Liu M, et al. Trends of incidence and prognosis of gastric neuroendocrine neoplasms: a study based on SEER and our multicenter research. Gastric Cancer. 2020;23(4):591-599. doi:10.1007/s10120-020-01046-8
Oviedo A, Luca R, Bestani C, et al. Argentinian registry of gastric neuroendocrine tumors: a closer look at type 1 [abstract C-17]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
Sok C, Ajay PS, Tsagkalidis V, Kooby DA, Shah MM. Management of gastric neuroendocrine tumors: a review. Ann Surg Oncol. 2023 Dec 7. doi:10.1245/s10434-023-14712-9
Song M, Camargo MC, Katki HA, et al. Association of antiparietal cell and anti-intrinsic factor antibodies with risk of gastric cancer. JAMA Oncol. 2022;8(2):268-274. doi:10.1001/jamaoncol.2021.5395
Song Y, Chen E, Chiang YS, et al. Classification of gastric neuroendocrine tumors and associations with survival [abstract 597]. Abstract presented at: 2024 American Society of Clinical Oncology Gastrointestinal Cancers Symposium; January 18-20, 2024; San Francisco, CA.
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American Society of Clinical Oncology.