Oncology
Gastroenteropancreatic Neuroendocrine Tumors
Peptide Receptor Radionuclide Therapy for Neuroendocrine Neoplasms
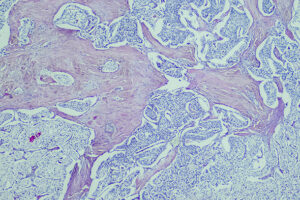
Peptide receptor radioligand therapy (PRRT) has an established role in the treatment of advanced somatostatin receptor (SSTR)–positive gastroenteropancreatic neuroendocrine tumors (GEP-NETs). At the 2024 ASCO Gastrointestinal Cancers Symposium, researchers shared preliminary data from the NETTER-2 trial, which is investigating the early use of PRRT in patients with newly diagnosed, advanced, grade 2 (G2) and grade 3 (G3), well-differentiated, SSTR-positive GEP-NETs.
Following this presentation, featured expert Jonathan R. Strosberg, MD, was interviewed by Conference Reporter Editor-in-Chief Tom Iarocci, MD. Dr Strosberg’s clinical perspectives on these findings are presented here.
PRRT incorporating somatostatin analogues (SSAs) as the ligand got its start in NETs with work by individuals such as Eric Krenning, MD, PhD, FRCP, in the Netherlands, who pioneered octreotide scintigraphy to image SSTR-expressing tumors. Over the years, more sophisticated scans (eg, dotatate positron emission tomography scans) have been developed. We have also learned that, by replacing the diagnostic radionuclide with a cytotoxic isotope such as yttrium-90 or lutetium-177, one can actually target cancer cells and either shrink or stabilize tumors. The concept of theranostics, or combining therapy and diagnostics, developed and grew out of this early work by Dr Krenning and others.
Today, we have a number of therapies for advanced GEP-NETs, and we are trying to learn more about their optimal sequencing. Very few active therapies have been compared head-to-head, and the activity of these treatments may differ somewhat based on the primary site. Tumoral SSTR expression is one of several considerations when looking at treatment options, and SSTR positivity is critical when it comes to PRRT.
NETTER-1 was the first phase 3 study of PRRT, and it evaluated the activity of lutetium Lu 177 dotatate (177Lu-dotatate). Patients in this study had midgut NETs that had progressed on standard-dose octreotide. They were randomly assigned to receive intravenous 177Lu-dotatate 7.4 GBq (200 mCi) every 8 weeks (4 cycles) plus intramuscular, long-acting octreotide 30 mg (177Lu-dotatate group) or high-dose, long-acting octreotide 60 mg every 4 weeks (control group). Data from NETTER-1 laid the foundation for the approval of 177Lu-dotatate for small-bowel NETs and other GEP-NETs, such as pancreatic, gastroduodenal, and rectal NETs. Until now, standard clinical practice has been to wait, at the very least, until progression on the SSA before considering PRRT.
At the 2024 ASCO Gastrointestinal Cancers Symposium, Simron Singh, MD, MPH, FRCPC, and colleagues presented the preliminary results from the phase 3 NETTER-2 trial (abstract LBA588). NETTER-2 is a somewhat complicated trial to interpret. It examined patients with well-differentiated but relatively high-grade (Ki-67 index of 10% to 55%) GEP-NETs. Recall that lower-grade NETs are more common overall, so NETs with a Ki-67 of 1% to 9% are much more common than those at 10% to 20%, which, in turn, are more common than those in the range of 20% to 50%. In addition, high-grade pancreatic NETs are more common than high-grade small-bowel NETs.
NETTER-2, then, evaluated first-line treatment in patients with relatively aggressive gastroenteric and pancreatic NETs, based on their grade. It would not really make sense to use 177Lu-dotatate early on in a patient with a low-grade tumor who can do very well for a very long time with SSA therapy. On the other hand, it seems likely that SSAs might not work as well in patients with a Ki-67 above 10%. To be clear, we really have very little data with SSAs (at any dose) once the Ki-67 gets above 10%. And so, this was an opportunity to study 177Lu-dotatate as a first-line drug in this more aggressive setting. Patients in NETTER-2 had a Ki-67 of 10% to 55%, and they were randomized in a 2:1 fashion to 177Lu-dotatate for 4 cycles combined with standard-dose octreotide vs high-dose octreotide in the control arm. The primary end point was progression-free survival (PFS), as it is in almost all phase 3 NET trials.
Not surprisingly, the trial was positive, with a median PFS of 22.8 months with 177Lu-dotatate vs 8.5 months with high-dose octreotide. The stratified hazard ratio was approximately 0.28, and this was highly statistically significant. The response rate was also quite high in the 177Lu-dotatate arm, at 43% vs approximately 9% in the comparator arm. That is much higher compared with what we saw in the NETTER-1 study. Perhaps this is related to NETTER-2 being a first-line study, or because pancreatic NETs generally have higher response rates to PRRT, and slightly more than half of the cases in NETTER-2 were pancreatic NETs. It is also possible that higher proliferative activity corresponds to a higher response rate. In terms of safety, there would not be any expectation of new toxicities in NETTER-2. Quality-of-life measures were the same between arms, which is more of a neutral finding and is not particularly positive or negative.
How might this impact clinical practice? If you look at the standard of care for SSTR-positive, well-differentiated, higher-grade G2 and G3 NETs, there are currently a number of options that one could consider, including SSAs alone as a first-line treatment. However, there is not a clearly established standard of care for well-differentiated G3 NETs. SSAs are a reasonable option for some patients with high G2 and G3 NETs, but, in my view, their use is less reasonable as the Ki-67 index increases. Other options include everolimus, sunitinib, and chemotherapy regimens such as capecitabine plus temozolomide. These drugs have primarily been studied in G1 and G2 tumors (Ki-67 <20%), although there are retrospective data in tumors with a Ki-67 of greater than 20%, particularly with chemotherapy.
As a result of NETTER-2, we now have strong data indicating that 177Lu-dotatate is a reasonable first-line option. However, it is also true that 177Lu-dotatate carries more risks than octreotide. Octreotide is among the most benign drugs that can be given in any type of cancer. So, I think that NETTER-2 begs the question of whether it is advisable to start immediately with 177Lu-dotatate, which is associated with a much longer PFS but definitely has risks, or to start with octreotide or lanreotide, which have almost no risks. It is really a sequencing question, and answering the sequencing question ideally requires overall survival (OS) data, which we do not have. All of our NET studies are very underpowered to assess impact on OS; nevertheless, I think that it would be nice to see at least a trend toward improved OS with first-line 177Lu-dotatate. We await that information.
NETTER-2 gives legitimacy to patients and physicians who want to start treatment early with PRRT rather than waiting until progression on SSA therapy. Although SSA therapy is probably still appropriate as first-line treatment for some patients with a Ki-67 of greater than 10%, factors favoring first-line PRRT include high tumor or symptom burden and evidence of rapid progression if there are 2 scans to compare over time. In these circumstances, it may be a good idea to get nuclear medicine involved at the very outset rather than waiting until progression on SSA therapy.
Del Rivero J, Perez K, Kennedy EB, et al. Systemic therapy for tumor control in metastatic well-differentiated gastroenteropancreatic neuroendocrine tumors: ASCO guideline. J Clin Oncol. 2023;41(32):5049-5067. doi:10.1200/JCO.23.01529
Grawe F, Ebner R, Geyer T, et al. Validation of the SSTR-RADS 1.0 for the structured interpretation of SSTR-PET/CT and treatment planning in neuroendocrine tumor (NET) patients. Eur Radiol. 2023;33(5):3416-3424. doi:10.1007/s00330-023-09518-y
Harris PE, Zhernosekov K. The evolution of PRRT for the treatment of neuroendocrine tumors; what comes next? Front Endocrinol (Lausanne). 2022;13:941832. doi:10.3389/fendo.2022.941832
Levine R, Krenning EP. Clinical history of the theranostic radionuclide approach to neuroendocrine tumors and other types of cancer: historical review based on an interview of Eric P. Krenning by Rachel Levine. J Nucl Med. 2017;58(suppl 2):3S-9S. doi:10.2967/jnumed.116.186502
Singh S, Halperin DM, Myrehaug S, et al. [177Lu]Lu-DOTA-TATE in newly diagnosed patients with advanced grade 2 and grade 3, well-differentiated gastroenteropancreatic neuroendocrine tumors: primary analysis of the phase 3 randomized NETTER-2 study [abstract LBA588]. Abstract presented at: 2024 American Society of Clinical Oncology Gastrointestinal Cancers Symposium; January 18-20, 2024; San Francisco, CA.
Strosberg J, El-Haddad G, Wolin E, et al; NETTER-1 Trial Investigators. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125-135. doi:10.1056/NEJMoa1607427
Strosberg JR, Caplin ME, Kunz PL, et al. 177Lu-Dotatate plus long-acting octreotide versus high‑dose long-acting octreotide in patients with midgut neuroendocrine tumours (NETTER-1): final overall survival and long-term safety results from an open-label, randomised, controlled, phase 3 trial [published correction appears in Lancet Oncol. 2022;23(2):e59]. Lancet Oncol. 2021;22(12):1752-1763. doi:10.1016/S1470-2045(21)00572-6
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American Society of Clinical Oncology.