Oncology
Gastroenteropancreatic Neuroendocrine Tumors
Personalizing Therapy for Patients With Gastroenteropancreatic Neuroendocrine Tumors
The identification and validation of novel predictive biomarkers might enhance the ability to individualize treatment for neuroendocrine tumors (NETs). At the North American Neuroendocrine Tumor Society (NANETS) 2023 Multidisciplinary NET Medical Symposium, researchers presented updated data on potential biomarkers for NETs.
Following these presentations, featured expert Thorvardur R. Halfdanarson, MD, was interviewed by Conference Reporter Editor-in-Chief Tom Iarocci, MD. Dr Halfdanarson’s clinical perspectives on these findings are presented here.
Data from multiple countries around the world show an increase over time in both the incidence and the prevalence of NETs, which means that we will continue to have more patients with NETs living longer and requiring more medical attention and improved therapy options. Therefore, we will need continued additional resources directed to NET research, including clinical trials, and NET care in general to continue to move the field forward.
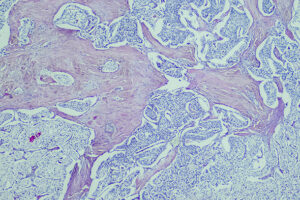
One important area where we are continuing our research is in the field of personalized therapy in gastroenteropancreatic NETs (GEP-NETs). I think that the high-level view of personalizing therapy is to do so based on the anatomic origin of disease and tumor grade. We know that, in terms of systemic therapy, different therapies work better against different NETs. For example, capecitabine plus temozolomide has excellent activity in pancreatic NETs, but not as much activity overall in small-bowel NETs.
To personalize therapy for patients with GEP-NETs further, there are a few things that we could look at. The first would be to gain a better understanding of the tumor genomics, as discussed in abstracts T-6 and B-3 from the NANETS 2023 Multidisciplinary NET Medical Symposium. We are barely scratching the surface. One example of the benefits of understanding tumor genomics can be found in patients with a rare genetic condition called von Hippel-Lindau disease (VHL). The HIF-2 alpha inhibitor belzutifan is an extremely effective therapy that works exceptionally well in the treatment of pancreatic NETs, specifically in patients with VHL. However, this genetic condition affects only a small minority of patients with pancreatic NETs.
For small-bowel NETs, we know that there are not a lot of recurrent genomic alterations. Although certain alterations are seen with more frequency than others, it does not appear to be the same few molecular alterations that occur regularly. However, research is continuing to identify potential novel alterations. A recently published genome-wide association study of 307 patients with small-bowel NETs and 287,137 controls from a Finnish registry found 4 new loci that were not previously reported, including 1 in a gene that is likely directly related to the differentiation of intestinal stem cells in the gut. This information is promising and deserves follow-up attention and research.
We have known for a number of years that well-differentiated tumors of grades 1, 2, or 3 that are avid on both fluorodeoxyglucose positron emission tomography (FDG PET) and dotatate PET are more aggressive than tumors that are positive only on dotatate or somatostatin receptor (SSTR) PET. And if tumors are only positive on FDG PET, they are likely to be more aggressive than those that are positive on SSTR PET. This information does not yet empirically change our treatment, but I could see future clinical trials being designed to look at both FDG and SSTR PET and using the results to help direct patients to a particular treatment based on PET avidity.
According to recent research, the peptide receptor radionuclide therapy (PRRT) predictive quotient (PPQ) appears to be a tool that may help predict individual patient responses to PRRT. If the test is positive, the patient is very likely to respond to PRRT. If the test is negative, they are not very likely to respond. These are early data from an interim analysis, so I think that we need a prospective clinical trial to validate these results before we adopt it in clinical practice. We also might be able to get information to help predict the toxicity of PRRT by looking at factors such as clonal hematopoiesis in patients before starting therapy, with Sonbol et al presenting their findings from their prospective study on clonal hematopoiesis in patients with NETs prior to lutetium Lu 177 dotatate therapy at the NANETS meeting (abstract O-9). In the future, we will hopefully be able to take predictors of treatment efficacy and predictors of toxicity and put them into a model to try to determine what will work best for that particular patient.
Overall, for most of the interventions that we use in our patients, we need better predictors and more reliable markers to provide optimal personalized therapy. There has been a lot of discussion about tumor markers such as chromogranin A (abstract O-5) and the NETest, among others. Although we have some data supporting the role of those markers, we do not yet have validated clinical trial data or information on how to apply them in the clinic. I could see a potential future role for these and other markers in determining how often to scan patients, but I think that we need better data and, ideally, to study these and other markers in the context of prospective clinical trials. For example, we need data showing that the markers have a positive impact on overall patient outcomes, such as survival and quality of life, and that they add value. If a tumor marker is not changing the overall outcome or is not providing information to help me guide individual patient therapy, I am not sure that it adds much value in a clinical setting.
Al-Toubah T, Morse B, Strosberg J. Efficacy of capecitabine and temozolomide in small bowel (midgut) neuroendocrine tumors. Curr Oncol. 2022;29(2):510-515. doi:10.3390/curroncol29020046
Bodei L, Raj N, Do RK, et al. Interim analysis of a prospective validation of 2 blood-based genomic assessments (PPQ and NETest) to determine the clinical efficacy of 177Lu-DOTATATE in neuroendocrine tumors. J Nucl Med. 2023;64(4):567-573. doi:10.2967/jnumed.122.264363
Das S, Dasari A. Epidemiology, incidence, and prevalence of neuroendocrine neoplasms: are there global differences? Curr Oncol Rep. 2021;23(4):43. doi:10.1007/s11912-021-01029-7
Giri AK, Aavikko M, Wartiovaara L, et al. Genome-wide association study identifies 4 novel risk loci for small intestinal neuroendocrine tumors including a missense mutation in LGR5. Gastroenterology. 2023;165(4):861-873. doi:10.1053/j.gastro.2023.06.031
Halfdanarson TR, Capdevila J, Halperin DM, et al. Genetic profiling in the randomized controlled phase 3 COMPOSE trial of 177Lu-edotreotide for well-differentiated aggressive grade 2/3 gastroenteropancreatic neuroendocrine tumors [abstract T-6]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
Meng Q, Halfdanarson TR, Bornhorst J, et al. Chromogranin a as surveillance biomarker in patients with carcinoids (CASPAR) [abstract O-5]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
Mohamed A, Asa SL, Lee Z, et al. The predictive impact of dual somatostatin receptor/fluorodeoxyglucose (FDG) positron emission tomography (PET) in metastatic gastroenteropancreatic neuroendocrine tumors (GEP-NETs): review of literature and a single institution experience. J Gastrointest Oncol. 2023;14(2):1087-1094. doi:10.21037/jgo-22-1011
Nunez JE, Bruce J, Danesh A, et al. Translational biomarkers in G2-3 NENs: analysis from NET-001 and NET-002 trials [abstract B-3]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
Pelle E, Al-Toubah T, Morse B, Strosberg J. Belzutifan in a patient with VHL-associated metastatic pancreatic neuroendocrine tumor. J Natl Compr Canc Netw. 2022;20(12):1285-1287. doi:10.6004/jnccn.2022.7047
Sonbol MB, Kusne Y, Lasho T, et al. Prevalence of clonal hematopoiesis (CH) in neuroendocrine tumor (NET) patients prior to lutetium 177 dotatate (Lu177): a prospective study [abstract O-9]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the North American Neuroendocrine Tumor Society.