Oncology
Gastroenteropancreatic Neuroendocrine Tumors
Potential Biomarkers in Gastroenteropancreatic Neuroendocrine Tumors
Biomarkers are an area of active research in gastroenteropancreatic neuroendocrine tumors (GEP-NETs). So far, years of research have yet to deliver clinically useful biomarkers for optimal therapeutic selection, ongoing patient monitoring, or predicting patient response to therapy. At the 2024 ASCO Gastrointestinal Cancers Symposium, researchers presented data on several potential biomarkers in GEP-NETs.
Following these presentations, featured expert Timothy J. Hobday, MD, was interviewed by Conference Reporter Editor-in-Chief Tom Iarocci, MD. Dr Hobday’s clinical perspectives on these findings are presented here.
Biomarkers that could help us select the therapies that are most likely to benefit our individual patients by predicting response or toxicity to therapy or, better yet, by improving our monitoring and prediction of recurrence or progression are something that we do not have yet, in my opinion. These biomarkers would, ideally, give us meaningful information that would improve our patients’ life span and quality of life (QOL).
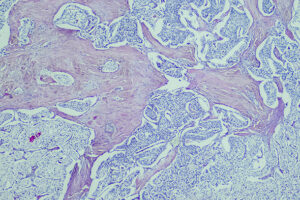
The biomarkers that are currently in our pathology reports mostly relate to the histologic differentiation of tumors, reported as well-differentiated vs poorly differentiated tumors and as Ki-67 expression. Ki-67 and some other biomarkers that are used to predict prognosis work pretty well when you look at large groups of patients and overall prognosis, but they are really poor predictors of what will happen to an individual patient or of the best initial therapeutic approach. For example, some patients who have well-differentiated grade 2 NETs with a Ki-67 of 15% can have tumors that behave as indolently as grade 1 tumors. There are also patients with well-differentiated grade 3 NETs and a Ki-67 of 28% who still have relatively indolent disease and may benefit from somatostatin analogue therapy.
Some biomarkers that have been used in the longitudinal management of patients or in the monitoring for recurrence, such as chromogranin A, neuron-specific enolase, and pancreastatin, are not very effective at helping us treat individual patients. They are neither sensitive nor specific, their values can fluctuate significantly from test to test, and, more importantly, there is no suggestion that following any biomarker and acting on changes could help us determine an optimal course of therapy or monitoring for each patient and increase patient confidence, life span, and QOL as a result.
The NETest is frequently touted as a better biomarker to monitor patients who are on therapy and to decide whether they are improving. However, the available data are not yet convincing to me that this has an additive benefit or that it can replace standard clinical evaluations and periodic imaging.
A developing area in the literature is trying to predict and document responses to peptide receptor radionuclide therapy (PRRT) in different patient groups. One serum biomarker that is being evaluated is the PRRT prediction quotient (PPQ). A retrospective analysis of a data set showed that the PPQ may help predict those who are more likely to benefit from PRRT. But I think that, until this is evaluated prospectively with control of many other clinical variables, it is difficult to know whether the PPQ is useful as a prognostic or predictive biomarker at this time. The PPQ also needs to be further evaluated to determine if it might be predictive of response to other therapies as well, not just PRRT.
As an aside on the safety of PRRT, we know that the most dreaded complication of PRRT is the chance of developing a treatment-related myeloid malignancy, either myelodysplastic syndromes (MDS) or acute leukemia. The NETTER-1 trial reported a 2% to 3% risk of MDS at 24 months, so these malignancies can threaten our patients’ lives sometimes well before when their NETs might. Our group at Mayo Clinic is looking at clonal hematopoietic mutations detected in genomic sequencing that potentially precede the development of myeloid malignancies. Our preliminary data showed that 45.9% of our patients with NETs had detectable clones before they had PRRT. So, I think that this is also a potential biomarker of importance, and we hope to grow our database to try to predict who might be at higher risk of MDS or acute leukemia in the first couple of years after treatment with PRRT.
We would also like to predict response to other therapies, such as chemotherapy, specifically with capecitabine plus temozolomide, which is generally our first-line regimen for pancreatic and other NETs. A loss of O6-methylguanine-DNA methyltransferase (MGMT) documented by either immunohistochemistry or promoter methylation has been thought to be a biomarker for increased response to therapy and, perhaps, duration of disease control or survival. But we have a lot of conflicting evidence.
There was an abstract at the 2024 ASCO Gastrointestinal Cancers Symposium touching on this (abstract 598), but the best data set is probably from the prospective randomized ECOG-ACRIN study E2211 comparing temozolomide alone with temozolomide plus capecitabine, which included a biomarker substudy. Although response rates were numerically higher in patients with a low expression of MGMT by immunohistochemistry and promoter methylation, MGMT expression was not found to be prognostic for progression-free or overall survival. So, this remains a biomarker that, perhaps, is not ready for standard use but that has accumulated data showing that it might predict response rates in patients using temozolomide. However, again, it may also be prognostic and not just predictive.
Although TKIs targeting the mTOR or VEGF receptor pathways are part of our usual treatment options for patients with NETs, we do not have a good way of choosing one over the other for an individual patient. I liked abstract 599 from the ASCO symposium evaluating whether we can use serum VEGFA levels to predict outcomes in a prospective phase 2 trial of the VEGF receptor inhibitor nintedanib. We know that there is an interplay between high levels of VEGF expression and an immunosuppressive tumor microenvironment. So, I think that this is a very interesting idea and that it could also help us explore the use of VEGF receptor inhibition to improve outcomes with immune checkpoint inhibition. While I do not think that this abstract proved anything, I do believe that it is representative of an interesting concept of trying to correlate serum biomarkers with our established therapies and to look for signals that may predict who will benefit.
Bevere M, Masetto F, Carazzolo ME, et al. An overview of circulating biomarkers in neuroendocrine neoplasms: a clinical guide. Diagnostics (Basel). 2023;13(17):2820. doi:10.3390/diagnostics13172820
Bodei L, Raj N, Do RK, et al. Interim analysis of a prospective validation of 2 blood-based genomic assessments (PPQ and NETest) to determine the clinical efficacy of 177Lu-DOTATATE in neuroendocrine tumors. J Nucl Med. 2023;64(4):567-573. doi:10.2967/jnumed.122.264363
Brage ET, Pérez JF, Martín LMN, et al. Prognostic value of O6-methylguanine-DNA methyltransferase (MGMT) status in pancreatic neuroendocrine tumors with capecitabine and temozolomide (CAPTEM) [abstract 598]. Abstract presented at: 2024 American Society of Clinical Oncology Gastrointestinal Cancers Symposium; January 18-20, 2024; San Francisco, CA.
Brighi N, Lamberti G, Andrini E, et al. Prospective evaluation of MGMT-promoter methylation status and correlations with outcomes to temozolomide-based chemotherapy in well-differentiated neuroendocrine tumors. Curr Oncol. 2023;30(2):1381-1394. doi:10.3390/curroncol30020106
Kunz PL, Graham NT, Catalano PJ, et al. Randomized study of temozolomide or temozolomide and capecitabine in patients with advanced pancreatic neuroendocrine tumors (ECOG-ACRIN E2211). J Clin Oncol. 2023;41(7):1359-1369. doi:10.1200/JCO.22.01013
Sonbol MB, Kusne Y, Lasho T, et al. Prevalence of clonal hematopoiesis (CH) in neuroendocrine tumor (NET) patients prior to lutetium 177 Dotatate (Lu177): a prospective study [abstract O-9]. Abstract presented at: North American Neuroendocrine Tumor Society 2023 Multidisciplinary NET Medical Symposium; October 4-6, 2023; Montreal, Quebec.
Sonti S, Wang K, Attwood K, et al. Potential biomarkers for treatment response in advanced non-pancreatic neuro-endocrine tumors [abstract 599]. Abstract presented at: 2024 American Society of Clinical Oncology Gastrointestinal Cancers Symposium; January 18-20, 2024; San Francisco, CA.
Strosberg JR, Caplin ME, Kunz PL, et al. 177Lu-Dotatate plus long-acting octreotide versus high-dose long-acting octreotide in patients with midgut neuroendocrine tumours (NETTER-1): final overall survival and long-term safety results from an open-label, randomised, controlled, phase 3 trial [published correction appears in Lancet Oncol. 2022;23(2):e59]. Lancet Oncol. 2021;22(12):1752-1763. doi:10.1016/S1470-2045(21)00572-6
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American Society of Clinical Oncology.