Rheumatology
Systemic Lupus Erythematosus
Novel Clinical Outcome Assessment Measures for Systemic Lupus Erythematosus
Novel outcome assessments were among the topics of interest at the 2023 Congress of Clinical Rheumatology (CCR) West. Work continues to improve these assessment tools and apply them in clinical trials, with the ultimate goal being remission for patients with systemic lupus erythematosus (SLE).
Following these proceedings, featured expert Anca D. Askanase, MD, MPH, was interviewed by Christopher Ontiveros, PhD. Dr Askanase’s clinical perspectives are presented here.
Several global disease activity measures are in use in clinical trials, including SLEDAI (SELENA-SLEDAI, the SLEDAI-2K, and the hybrid SELENA-SLEDAI), the BILAG index, and the PGA. These instruments generally assess SLE disease activity based on what has been happening with the patient over the past month, and they account for a wide range of lupus manifestations. None of the instruments are perfect. We rely on the PGA as an additional means of capturing the overall impact of disease activity. Composite measures are used to determine response to treatment in clinical trials. For example, therapeutic clinical trials rely on the SRI-4 and the BICLA index to gauge response to therapy.
There is great interest in refining disease activity measures and a strong desire to better understand how therapeutics impact disease activity in patients with lupus. A number of groups are working toward these goals. With the support of the Lupus Foundation of America (LFA), our team at Columbia University helped to develop a disease activity instrument called LFA-REAL (also known as the Lupus Foundation of America’s Rapid Evaluation of Activity in Lupus system). It has both physician and patient components. The evaluation of how active the disease is from the patient’s perspective is critical yet incompletely captured by the currently available patient-reported outcome measures that evaluate fatigue, quality of life, or mental health (depression and anxiety). The LFA-REAL also offers the option for physicians to add manifestations that are rare in lupus, such as ocular manifestations, to fully capture the complexity of SLE.
At CCR West, clinical outcome assessment measures were, of course, integral to many reports, and a presentation by Kenneth Kalunian, MD, summarized some of the challenges and opportunities in this area. Since the vast majority of patients with lupus have joint symptoms, there is particular interest in finding improved ways to quantify these symptoms, as we already do in patients with rheumatoid arthritis. Clinical trials have started to include assessments of the number of tender and swollen joints, with some studies showing improvements, but they are not as precise as we would like them to be. We began using musculoskeletal ultrasound imaging to assess lupus arthritis; the ultrasound evaluates hypervascularity, synovitis, and swelling, and, more recently, includes tenosynovitis to obtain a more complete picture of joint involvement in lupus. Additionally, optical imaging could be the next frontier in joint imaging. Optical tomography has been evaluated in patients with rheumatoid arthritis, and reports from our team and others have shown promising data in patients with lupus. These data are evolving, and we hope that, ultimately, we will be able to better diagnose and evaluate arthritis in lupus.
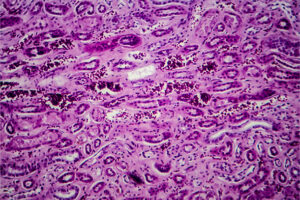
The presentation by Dr Kalunian illustrated the renewed attention to finding biomarkers that correlate with disease activity. Complement and DNA have long been used, but they are imperfect and imprecise in assessing disease activity. Interferon signatures as a means of predicting who will respond to treatment and measuring treatment response has sparked some interest. For patients with lupus nephritis, utilizing the definition of complete renal response (defined as a urinary protein to creatinine ratio <0.5 g/g, along with a stable serum creatinine) has been successful in therapeutic clinical trials, and it appears to be accurate in measuring improvement and discriminating in clinical trials.
We are not quite there yet. More work needs to be done, but we have made progress. The newer LLDAS and DORIS remission measures have been evaluated in several clinical trials, and the possibility of remission is quite extraordinary. This is the holy grail; getting to remission is what we strive to achieve. We need to understand how best to use the established and emerging therapeutics to decrease and quench disease activity and to achieve remission.
Askanase AD, Daly RP, Okado M, et al. Development and content validity of the Lupus Foundation of America Rapid Evaluation of Activity in Lupus (LFA-REAL™): a patient-reported outcome measure for lupus disease activity. Health Qual Life Outcomes. 2019;17(1):99. doi:10.1186/s12955-019-1151-8
Askanase AD, Tang W, Zuraw Q, Gordon R, Brotherton B, Merrill JT. Evaluation of the LFA-REAL clinician-reported outcome (ClinRO) and patient-reported outcome (PRO): prespecified analysis of the phase III ustekinumab trial in patients with SLE. Lupus Sci Med. 2023;10(1):e000875. doi:10.1136/lupus-2022-000875
Bruce IN, Furie RA, Morand EF, et al. Concordance and discordance in SLE clinical trial outcome measures: analysis of three anifrolumab phase 2/3 trials. Ann Rheum Dis. 2022;81(7):962-969. doi:10.1136/annrheumdis-2021-221847
Bruera S, Chavula T, Madan R, Agarwal SK. Targeting type I interferons in systemic lupus erythematous. Front Pharmacol. 2023;13:1046687. doi:10.3389/fphar.2022.1046687
Connelly K, Eades LE, Koelmeyer R, et al; TRM-SLE Consortium. Towards a novel clinical outcome assessment for systemic lupus erythematosus: first outcomes of an international taskforce. Nat Rev Rheumatol. 2023;19(9):592-602. doi:10.1038/s41584-023-00993-7
Ding H, Shen Y, Hong S-M, Xiang C, Shen N. Biomarkers for systemic lupus erythematosus – a focus on organ damage. Expert Rev Clin Immunol. 2023 Sep 15. doi:10.1080/1744666X.2023.2260098
Kalunian K. LUPUS in 2023: a new era. Oral presentation presented at: 2023 Congress of Clinical Rheumatology West; September 7-10, 2023; San Diego, CA.
Konieczny A, Kasenberg I, Mikołajczak A, Donizy P, Hałoń A, Krajewska M. Baseline proteinuria and serum creatinine concentration as clinical predictors of complete renal response in patients with lupus nephritis: a single-center experience. Int J Environ Res Public Health. 2022;19(23):15909. doi:10.3390/ijerph192315909
Marone A, Tang W, Kim Y, et al. Evaluation of SLE arthritis using frequency domain optical imaging. Lupus Sci Med. 2021;8(1):e000495. doi:10.1136/lupus-2021-000495
Morand EF, Abreu G, Furie RA, Golder V, Tummala R. Lupus low disease activity state attainment in the phase 3 TULIP trials of anifrolumab in active systemic lupus erythematosus. Ann Rheum Dis. 2023;82(5):639-645. doi:10.1136/ard-2022-222748
Parra Sánchez AR, van Vollenhoven RF, Morand EF, et al. Targeting DORIS remission and LLDAS in SLE: a review. Rheumatol Ther. 2023 Oct 5. doi:10.1007/s40744-023-00601-w
van Vollenhoven R, Askanase AD, Bomback AS, et al. Conceptual framework for defining disease modification in systemic lupus erythematosus: a call for formal criteria. Lupus Sci Med. 2022;9(1):e000634. doi:10.1136/lupus-2021-000634
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the Congress of Clinical Rheumatology.