Rheumatology
Systemic Lupus Erythematosus
Challenges in Systemic Lupus Erythematosus: Where Do We Stand?
Overview
Despite significant advances in the understanding of the pathophysiology of systemic lupus erythematosus (SLE), a number of challenges persist. In particular, researchers continue to grapple with the clinical and molecular heterogeneity of SLE. However, progress is occurring on a number of fronts.
What are some of the current challenges in SLE?
Joan T. Merrill, MD
|
|
“In ‘negative’ trials that report response rates in the range of 40% to 50% for patients who received placebo plus standard of care, it is difficult to know with certainty whether the investigational drug failed or not. That drug may work well in only 40% to 50% of patients, which is actually a good response rate in those with SLE.”
One of the major challenges in SLE is that successful phase 2 trials are often followed by failed phase 3 trials. There are a number of reasons for this, but some of them are related to the study design and a reduced ability to detect an efficacy signal. Sometimes, we do know that a drug has failed (eg, the response rates were low across the board and the study drug did not significantly improve response rates compared with the standard of care). However, in “negative” trials that report response rates in the range of 40% to 50% for patients who received placebo plus standard of care, it is difficult to know with certainty whether the investigational drug failed or not. That drug may work well in only 40% to 50% of patients, which is actually a good response rate in those with SLE. With such high placebo response rates, it is challenging for potentially useful drugs to demonstrate efficacy. In most lupus trials, patients in the placebo group are receiving significant background treatments as standard of care, which often includes corticosteroids. And, although steroids are effective, the long-term use of steroids, even at lower doses, carries risks. So, we are dampening our ability to detect efficacy while using treatments with unacceptable side effects. Clinical studies are beginning to limit background therapies or to taper the corticosteroid dose to reduce the high response rates observed in the standard-of-care-plus-placebo group, which is a step in the right direction.
Biomarkers in SLE continue to be a challenge, but we are making progress, as reported in the paper by Guthridge et al. A machine learning approach was applied to extensive gene expression, soluble mediator, autoantibody, and clinical information in a large cohort of patients whose SLE had been well characterized clinically. Seven biomarker-based phenotypic clusters of adult patients with SLE became discernable that were not apparent from the clinical information. While using molecular subsets alone will not resolve all problems in the interpretation of lupus trials, this type of profiling is promising.
Bevra H. Hahn, MD
|
|
“Despite treatment with the available therapies, however, there are still patients with uncontrolled skin manifestations of SLE. Some of the clinical trials today specifically focus on CLE, which is a positive development in my view, since this seems to be a different subset of patients.”
I would agree with Dr Merrill on the challenges with available biomarkers. We need better biomarkers to predict disease prognosis, disease remission, and long-term adverse events in SLE. Laboratory results from a standard clinic cannot identify patients who will experience flares and who will respond to treatment. Thus, the reliable identification of the right treatment for the right patient currently remains a challenge in SLE.
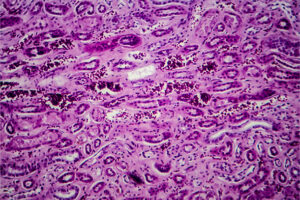
In addition, when I think of challenges that might be more specific to lupus, some of the dermatologic manifestations come to mind. Cutaneous manifestations encompass a broad spectrum of findings that can occur with systemic involvement and can occur independent of SLE. The rash from acute cutaneous lupus erythematosus (CLE) generally responds to treatment for the whole systemic disease, but chronic CLE may be more of a problem. Fortunately, patients with more severe chronic CLE are less likely to have significant systemic involvement, and there are a number of ways to focus on the skin, including several topical therapies that are available for the treatment of these skin manifestations and steroid injections that specifically are used for joint symptoms and skin manifestations. Additionally, there are systemic treatments that seem to be more effective for skin manifestations than for other manifestations of the disease.
Despite treatment with the available therapies, however, there are still patients with uncontrolled skin manifestations of SLE. Some of the clinical trials today specifically focus on CLE, which is a positive development in my view, since this seems to be a different subset of patients.
George C. Tsokos, MD
|
|
“Moving across the disease spectrum, there can be crosstalk between the skin and other organs such as the kidney. For example, inflamed neutrophils from the skin may go to the kidney to start the inflammatory process, similar to a pigeon transferring the fire from one place to another.”
To add to Dr Hahn’s comments on the skin manifestations of SLE, it is essential to acknowledge the complicated and complex nature of the process. As she noted, there are forms of CLE that are limited to the skin and do not result in systemic manifestations. Then, moving across the disease spectrum, there can be crosstalk between the skin and other organs such as the kidney, as discussed in the paper by Kolios et al. For example, inflamed neutrophils from the skin may go to the kidney to start the inflammatory process, similar to a pigeon transferring the fire from one place to another. Additionally, there are aspects of the pathophysiology that underlie cutaneous pathology that may differ from those involved in the development of inflammation in other organs. Perhaps due to such phenomena, treating SLE with a tumor necrosis factor inhibitor may improve skin involvement and worsen kidney inflammation. Thus, it is important to identify relevant subsets prior to conducting clinical trials, and it is equally important to remember that a “one-treatment-fits-all” approach in SLE is not a therapeutic reality.
Another challenge in SLE management relates to the prevention of flares and damage that may occur while reducing or withdrawing glucocorticoids. Current guidelines recommend using the lowest glucocorticoid dosage needed to control disease, with withdrawal of glucocorticoid therapy, as possible. This is an excellent goal, but, unfortunately, a complete withdrawal is not always feasible without relapse; maintenance with long-term 5 mg of prednisone in patients with inactive SLE can help prevent relapse, as shown by Mathian et al.
References
Borucki R, Werth VP. Expert perspective: an evidence-based approach to refractory cutaneous lupus erythematosus. Arthritis Rheumatol. 2020;72(11):1777-1785. doi:10.1002/art.41480
Dall’Era M, Bruce IN, Gordon C, Manzi S, McCaffrey J, Lipsky PE. Current challenges in the development of new treatments for lupus. Ann Rheum Dis. 2019;78(6):729-735. doi:10.1136/annrheumdis-2018-214530
Deng G-M, Tsokos GC. Pathogenesis and targeted treatment of skin injury in SLE. Nat Rev Rheumatol. 2015;11(11):663-669. doi:10.1038/nrrheum.2015.106
Dörner T, Furie R. Novel paradigms in systemic lupus erythematosus. Lancet. 2019;393(10188):2344-2358. doi:10.1016/S0140-6736(19)30546-X
European League Against Rheumatism. RheumaMap. A research roadmap to transform the lives of people with rheumatic and musculoskeletal diseases. Accessed June 2, 2021. https://www.eular.org/myUploadData/files/Rheuma_Map_A4_document_23_05_17.pdf
Felten R, Sagez F, Gavand P-E, et al. 10 most important contemporary challenges in the management of SLE. Lupus Sci Med. 2019;6(1):e000303. doi:10.1136/lupus-2018-000303
Guthridge JM, Lu R, Tran LT-H, et al. Adults with systemic lupus exhibit distinct molecular phenotypes in a cross-sectional study. EClinicalMedicine. 2020;20:100291. doi:10.1016/j.eclinm.2020.100291
Kolios AGA, Tsokos GC. Skin-kidney crosstalk in SLE. Nat Rev Rheumatol. 2021;17(5):253-254. doi:10.1038/s41584-021-00588-0
Mathian A, Pha M, Haroche J, et al. Withdrawal of low-dose prednisone in SLE patients with a clinically quiescent disease for more than 1 year: a randomised clinical trial. Ann Rheum Dis. 2020;79(3):339-346. doi:10.1136/annrheumdis-2019-216303
Petty AJ, Floyd L, Henderson C, Nicholas MW. Cutaneous lupus erythematosus: progress and challenges. Curr Allergy Asthma Rep. 2020;20(5):12. doi:10.1007/s11882-020-00906-8
Piga M, Arnaud L. The main challenges in systemic lupus erythematosus: where do we stand? J Clin Med. 2021;10(2):243. doi:10.3390/jcm10020243
Robert M, Miossec P. Interleukin-17 and lupus: enough to be a target? For which patients? Lupus. 2020;29(1):6-14. doi:10.1177/0961203319891243
Touma Z, Gladman DD. Current and future therapies for SLE: obstacles and recommendations for the development of novel treatments. Lupus Sci Med. 2017;4(1):e000239. doi:10.1136/lupus-2017-000239
Wallace DJ, Furie RA, Tanaka Y, et al. Baricitinib for systemic lupus erythematosus: a double-blind, randomised, placebo-controlled, phase 2 trial [published correction appears in Lancet. 2018;392(10146):476]. Lancet. 2018;392(10143):222-231. doi:10.1016/S0140-6736(18)31363-1