Rheumatology
Systemic Lupus Erythematosus
Addressing Refractory Systemic Lupus Erythematosus
Overview
The treatment of refractory systemic lupus erythematosus (SLE) is challenging. Data on the role of newer therapeutic agents and how they can best be incorporated into a new SLE treatment paradigm were presented at the recent 2023 Congress of Clinical Rheumatology (CCR) East.
Following these proceedings, featured expert Anca D. Askanase, MD, MPH, was interviewed by Christopher Ontiveros, PhD. Dr Askanase’s clinical perspectives are presented here.
Anca D. Askanase, MD, MPH
|
|
Michelle Petri, MD, MPH, presented one of the most interesting SLE treatment–related sessions at CCR East on the concept of disease modification in patients with lupus. We are very fortunate to have 2 additional novel therapeutics that were recently approved by the US Food and Drug Administration: anifrolumab for the treatment of SLE and voclosporin for the treatment of lupus nephritis. In addition, belimumab has recently received an expanded approval for adult and pediatric lupus nephritis.
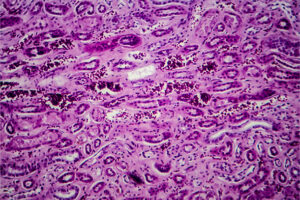
Currently, for patients with lupus nephritis, most physicians are administering mycophenolate plus steroids first before introducing one of these newer therapies, which are typically used as add-on therapies for refractory disease. Thus, there is some reluctance to start triple therapy with a steroid, mycophenolate, and belimumab or voclosporin from day 1. But perhaps we need to reconsider the way in which we are treating new-onset lupus nephritis, because the data suggest that the quicker we achieve complete renal response and resolved proteinuria, the more likely we are to preserve kidney function. Every episode of lupus nephritis is a hit on nephrons, and, over time, this translates into a decrease in the ability of the kidneys to last a patient's lifetime.
None of the clinical trial data to date suggest significant safety concerns for any of the new medications, so the paradigm may need to be shifted to introduce advanced therapies earlier. Patients and investigators are wondering how effective combination therapy that incorporates new agents will be for those who have failed with more traditional approaches to the treatment of lupus nephritis. Guideline recommendations for lupus nephritis are currently being updated, and this will hopefully provide some additional guidance to clinicians regarding patient management.
Data from the TULIP-1 and the TULIP-2 trials also showed that anifrolumab is effective in treating overall disease activity in SLE. In fact, the results demonstrated that anifrolumab provided a reduction in disease activity while also permitting the tapering of glucocorticoid therapy. In TULIP-2, the percentage of patients who had a British Isles Lupus Assessment Group–based Composite Lupus Assessment response at week 52 was approximately 48% in the anifrolumab group and 31.5% in the placebo group. Secondary end points with respect to decreases in the glucocorticoid dose also significantly favored anifrolumab, and the differences between treatment and placebo were even greater in the long-term extension phase. The long-term extension was unique in that it included a built-in placebo group, and the value of this large data set that includes both safety and efficacy is quite extraordinary. Notably, approximately 90% of patients in the treatment arm were taking 7.5 mg or less per day of prednisone at the end of the study, and 36% were able to completely stop steroid therapy. The potential steroid-sparing effects of these new biologics will hopefully allow physicians to be more comfortable and more aggressive with tapering steroid therapy. In addition, the increased risk of infections such as herpes zoster and herpes simplex virus that was observed with anifrolumab in the initial randomized controlled portion of the trial decreased over the course of the long-term extension phase and was similar to that of placebo, providing reassuring longer-term safety data.
Another important concept that was discussed during Dr Petri's lecture at CCR East was related to the evaluation of type 1 vs type 2 symptoms in patients with lupus. Understanding and classifying these symptoms can help clinicians better relate and communicate with their patients regarding their symptoms and can help facilitate a more effective treatment plan. Type 1 symptoms include those that are clearly related to inflammation and are most likely to respond to immune-modulatory and suppressive therapies, whereas type 2 symptoms are typically more vague, chronic, and less likely to be inflammatory in nature. Examples of type 2 symptoms include fatigue, diffuse pain, brain fog, cognitive dysfunction, sleep disturbances, and anxiety or depression. Understanding the type of symptoms that a patient is experiencing can be helpful when determining appropriate therapy and assessing therapeutic response.
While there are no specific clinical trial data on the use of these new biologics in the refractory setting, these therapeutic agents are already being considered when patients fail to respond to mycophenolate and corticosteroids. It is an exciting time, and I think that we are in a fortunate situation in which we have a lot more therapeutic options for the treatment of lupus than we have had for a long time.
References
Furie RA, Morand EF, Bruce IN, et al. Type I interferon inhibitor anifrolumab in active systemic lupus erythematosus (TULIP-1): a randomised, controlled, phase 3 trial. Lancet Rheumatol. 2019;1(4):e208-e219. doi:10.1016/S2665-9913(19)30076-1
Furie R, Morand EF, Askanase AD, et al. Anifrolumab reduces flare rates in patients with moderate to severe systemic lupus erythematosus. Lupus. 2021;30(8):1254-1263. doi:10.1177/09612033211014267
Furie R, Rovin BH, Houssiau F, et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med. 2020;383(12):1117-1128. doi:10.1056/NEJMoa2001180
Jayne D, Rovin B, Mysler EF, et al. Phase II randomised trial of type I interferon inhibitor anifrolumab in patients with active lupus nephritis. Ann Rheum Dis. 2022;81(4):496-506. doi:10.1136/annrheumdis-2021-221478
Kalunian KC, Furie R, Morand EF, et al. A randomized, placebo-controlled phase III extension trial of the long-term safety and tolerability of anifrolumab in active systemic lupus erythematosus. Arthritis Rheumatol. 2023;75(2):253-265. doi:10.1002/art.42392
Morand EF, Furie R, Tanaka Y, et al; TULIP-2 Trial Investigators. Trial of anifrolumab in active systemic lupus erythematosus. N Engl J Med. 2020;382(3):211-221. doi:10.1056/NEJMoa1912196
Petri M. Comparison of new therapies for SLE. Presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Pisetsky DS, Clowse MEB, Criscione-Schreiber LG, Rogers JL. A novel system to categorize the symptoms of systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2019;71(6):735-741. doi:10.1002/acr.23794
Rovin BH, Solomons N, Pendergraft WF 3rd, et al; AURA-LV Study Group. A randomized, controlled double-blind study comparing the efficacy and safety of dose-ranging voclosporin with placebo in achieving remission in patients with active lupus nephritis. Kidney Int. 2019;95(1):219-231. doi:10.1016/j.kint.2018.08.025
Rovin BH, Teng YKO, Ginzler EM, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial [published correction appears in Lancet. 2021;397(10289):2048]. Lancet. 2021;397(10289):2070-2080. doi:10.1016/S0140-6736(21)00578-X
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the Congress of Clinical Rheumatology.