Rheumatology
Systemic Lupus Erythematosus
Autoimmunity and Autoantibody Profiles in Systemic Lupus Erythematosus
Overview
Systemic lupus erythematosus (SLE) is a prototypical autoimmune disease with many associated autoantibodies. Information on the role of autoimmunity and autoantibody profiles in SLE was presented at the 2023 Congress of Clinical Rheumatology (CCR) West.
Following these proceedings, featured expert Vasileios C. Kyttaris, MD, was interviewed by Christopher Ontiveros, PhD. Clinical perspectives from Dr Kyttaris are presented here.
Vasileios C. Kyttaris, MDAssistant Professor of Medicine |
|
“ . . . although the correlation is not one-to-one, there is a very strong association between the presence of certain autoantibodies and certain disease manifestations.”
SLE is regarded as the prototypic autoimmune disease with more than 100 autoantibodies that have been identified in patients with this disease. These antibodies target a variety of antigens, typically ones that are associated with either the DNA itself (ie, double-stranded DNA [dsDNA]) or the machinery of transcription or translation. Notably, the presence of certain autoantibodies can be used to categorize patients into specific phenotypes. Further, although the correlation is not one-to-one, there is a very strong association between the presence of certain autoantibodies and certain disease manifestations.
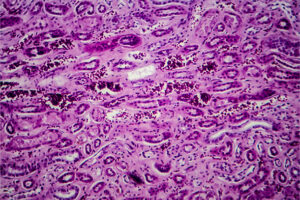
For example, one of the most commonly identified autoantibodies is the anti-dsDNA antibody, which is well known to be correlated with the development of lupus nephritis (LN). Not only is there the correlation, but these autoantibodies appear to be directly or indirectly involved in the pathogenic process of LN, including the formation of immune complexes that are deposited in the kidneys and initiate the inflammatory cascade. This is what leads to renal inflammation and, ultimately, with continued worsening over time, renal failure. Anti-dsDNA antibody levels are also correlated with disease activity. The correlation is not perfect in that we cannot say that a patient with rising levels will certainly experience a flare, but levels generally increase during exacerbations and decrease during periods of quiescence.
There are other autoantibodies that may also be helpful to identify in SLE. The anti-Smith (Sm) antibody has been associated with the development of more severe disease, especially LN and other renal complications. A higher frequency of anti-Sm antibodies in African American patients with SLE has been described. The anti-Ro antibody has been linked to photosensitivity and pregnancy-related complications, such as complete heart block in the fetus. SLE has also been associated with the presence of antiphospholipid (aPL) antibodies that are correlated with an increased risk of thrombosis. Finally, the anti-ribonucleoprotein (RNP) antibody is often associated with a milder form of lupus called mixed connective tissue disease.
In a presentation at CCR West, Karen Costenbader, MD, MPH, discussed the temporal progression of autoantibody specificities and the development of clinical SLE. She reviewed a classic study from 20 years ago showing that healthy military recruits who developed SLE had evidence of autoantibodies several years prior to a clinical diagnosis of SLE. These individuals demonstrated a progressive accumulation of autoantibodies over time. The antinuclear antibodies (ANA) and the anti-Ro antibodies tended to appear in the serum earlier on, and then antibodies such as anti-RNP, anti-Sm, and anti-dsDNA appeared later. This expansion of autoantibody specificity spectrum, termed epitope spreading, starts with a break in tolerance against a specific autoantigen that becomes more exuberant over time as more autoantigens are recognized by the immune system as being foreign.
This process is highly variable and is not necessarily unique to SLE. Notably, prior to the development of clinical SLE (or other autoimmune conditions), patients may exhibit nonspecific symptoms (eg, joint pain or myalgia) and have some evidence of autoimmunity (eg, positive ANA or ≥1 specific autoantibodies). This condition is referred to as undifferentiated connective tissue disease or pre-lupus. The presence or absence of specific autoantibodies can be helpful in these patients. For example, for someone who has a positive ANA test, along with being positive for antibodies such as anti-dsDNA or anti-Sm, the likelihood of them developing SLE is much higher compared with those who do not have those antibodies. Nonetheless, the study of preclinical or early clinical autoimmunity is ongoing, and much remains unknown, including strategies to prevent progression to a clinical autoimmune disease.
Once you make the diagnosis of lupus, the autoantibodies do inform your approach in important ways. Since it has been demonstrated that those with anti-dsDNA antibodies are at a high risk for LN, we will follow such patients closely and measure the urine protein. Similarly, women with anti-Ro antibodies should be counseled regarding the risk of fetal congenital heart block if they become pregnant, while those with anti-aPL antibodies should be counseled about the risk of both recurrent spontaneous abortion and thrombosis. And, finally, if someone is positive for anti-RNP antibodies, we will follow and monitor them for the development of Raynaud’s disease, sclerodactyly, or even pulmonary hypertension.
The factors that lead to the development of SLE are thought to be both genetic and environmental. Dr Costenbader extensively discussed the environmental factors that influence the risk of developing SLE as we are trying to understand the process that leads from the initial break of immunologic tolerance to the development of preclinical autoimmunity and, eventually, clinical disease. Specifically, increased exposure to estrogens (either endogenous such as early menarche or exogenous such as oral contraceptive medications or postmenopausal hormone replacement) is associated with a modest increase in the risk of developing SLE. For example, the odds of developing SLE in women who take oral contraceptive medications are 1.5 times greater than the odds of developing SLE if the individual never took these medications. Smoking also modestly increases the odds of developing SLE, especially SLE with positive anti-dsDNA antibodies, which, as mentioned above, is associated with more severe forms of the disease (ie, LN). This association seems to disappear 5 years after smoking cessation, which is in line with other smoking-associated illnesses. Besides smoking, silica exposure may predispose one to SLE, with the odds for SLE development being as high as 4.6 times when exposed to high levels of silica over prolonged periods of time versus individuals who were never exposed.
Moreover, Dr Costenbader discussed the effect of diet on the development of SLE. Interestingly, obesity, which can exacerbate systemic inflammation, at age 18 years has been linked to the development of SLE later in life. When looking at specific ingredients in the diet, the increased consumption of ultra-processed foods has a very modest association with the development of SLE, while moderate alcohol intake may decrease the risk of SLE.
In conclusion, Dr Costenbader analyzed the effects of endogenous and exogenous factors outside the immune system that, by increasing systemic inflammation, may lead, likely in conjunction with genetic factors, to the development of systemic autoimmune diseases in general and SLE in particular.
References
Arbuckle MR, McClain MT, Rubertone MV, et al. Development of autoantibodies before the clinical onset of systemic lupus erythematosus. N Engl J Med. 2003;349(16):1526-1533. doi:10.1056/NEJMoa021933
Arroyo-Ávila M, Santiago-Casas Y, McGwin G Jr, et al. Clinical associations of anti-Smith antibodies in PROFILE: a multi-ethnic lupus cohort. Clin Rheumatol. 2015;34(7):1217-1223. doi:10.1007/s10067-015-2941-y
Caielli S, Wan Z, Pascual V. Systemic lupus erythematosus pathogenesis: interferon and beyond. Annu Rev Immunol. 2023;41:533-560. doi:10.1146/annurev-immunol-101921-042422
Choi MY, Chen I, Clarke AE, et al. Machine learning identifies clusters of longitudinal autoantibody profiles predictive of systemic lupus erythematosus disease outcomes. Ann Rheum Dis. 2023;82(7):927-936. doi:10.1136/ard-2022-223808
Choi MY, Costenbader KH. Understanding the concept of pre-clinical autoimmunity: prediction and prevention of systemic lupus erythematosus: identifying risk factors and developing strategies against disease development. Front Immunol. 2022;13:890522. doi:10.3389/fimmu.2022.890522
Costenbader KH. Pre-clinical autoimmunity: identifying risk factors & developing strategies against disease development in SLE. Oral presentation presented at: 2023 Congress of Clinical Rheumatology West; September 7-10, 2023; San Diego, CA.
Dema B, Charles N. Autoantibodies in SLE: specificities, isotypes and receptors. Antibodies (Basel). 2016;5(1):2. doi:10.3390/antib5010002
Pepmueller PH. Undifferentiated connective tissue disease, mixed connective tissue disease, and overlap syndromes in rheumatology. Mo Med. 2016;113(2):136-140.
Rekvig OP. The dsDNA, anti-dsDNA antibody, and lupus nephritis: what we agree on, what must be done, and what the best strategy forward could be. Front Immunol. 2019;10:1104. doi:10.3389/fimmu.2019.01104
Sherer Y, Gorstein A, Fritzler MJ, Shoenfeld Y. Autoantibody explosion in systemic lupus erythematosus: more than 100 different antibodies found in SLE patients. Semin Arthritis Rheum. 2004;34(2):501-537. doi:10.1016/j.semarthrit.2004.07.002
van Beers JJBC, Schreurs MWJ. Anti-Sm antibodies in the classification criteria of systemic lupus erythematosus. J Transl Autoimmun. 2022;5:100155. doi:10.1016/j.jtauto.2022.100155
Wang X, Xia Y. Anti-double stranded DNA antibodies: origin, pathogenicity, and targeted therapies. Front Immunol. 2019;10:1667. doi:10.3389/fimmu.2019.01667
Yoshimi R, Ueda A, Ozato K, Ishigatsubo Y. Clinical and pathological roles of Ro/SSA autoantibody system. Clin Dev Immunol. 2012;2012:606195. doi:10.1155/2012/606195
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the Congress of Clinical Rheumatology.