Rheumatology
Systemic Lupus Erythematosus
Conference Highlights: Toward Disease Modification in Systemic Lupus Erythematosus
With the availability of multiple potent and effective treatment options, disease modification is being discussed as an emerging and achievable goal in systemic lupus erythematosus (SLE). Several presentations at ACR Convergence 2023 addressed this critical issue.
Following these proceedings, featured expert Anca D. Askanase, MD, MPH, was interviewed by Christopher Ontiveros, PhD. Dr Askanase’s clinical perspectives on this topic are presented here.
ACR Convergence 2023 was an exciting meeting for advancements in lupus, as there were a lot of data presented supporting possible changes in the treatment paradigm and improvements in our ability to take care of patients, including the potential for disease modification and even disease remission.
In my presentation at the meeting (titled “Can Current Lupus Treatments Be Classified as DMALDs?”), I described our task force of experts from across the world who were recently convened to develop a conceptual framework for defining disease modification in SLE. We reviewed the literature on disease modification in many disease states, including in other areas of rheumatology, and we identified the themes that should be included in the definition of disease modification, such as minimizing disease activity and changing the course or progression of the disease. The current working definition of disease modification in patients with SLE is minimizing disease activity with the least treatment-associated drug toxicity and changing the progression of the disease. Our ability to create this framework is driven by the increased availability of multiple potent and effective therapies and by the availability of measures of disease activity.
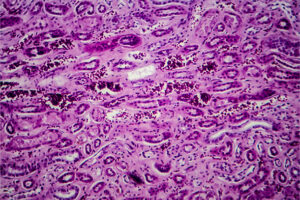
Our proposed matrix for the evaluation of disease modification highlights the need to include the element of time when assessing disease modification. We have divided the outcomes that are associated with disease modification in SLE into 3 eras: (1) in the first year, achieving the outcomes of decreasing disease activity, flares, and steroid use; (2) in years 2 to 5, sustaining reductions in disease activity, preventing flares, and continuing reductions in steroids and/or immunosuppressants, if possible; and (3) over 5 years, achieving long-term confirmation of disease modification, where the most important parameters are either no change or delayed progression in organ damage in nonrenal disease, and, in patients with renal disease, a decreased decline in glomerular filtration rate and a decreased risk of chronic kidney disease.
I think that it has become clear over the past 2 decades that long-term steroid use plays a role in the damage accrual that is seen in patients with SLE. Early on in the disease course, the main driver of damage is the disease activity itself, but further down the line, much of the damage accumulation is related to long-term steroid exposure and the cumulative steroid dose. So, it has become clear that, to truly modify the disease course, we need to minimize steroid exposure, both up front and long-term. The most recent European Alliance of Associations for Rheumatology (EULAR) recommendations for the management of SLE are clear about the need to minimize steroid use in SLE and about how using other therapies, including newer biologics, earlier may help to achieve disease modification earlier and minimize steroid exposure. It is important to recognize that one of the main ways to minimize steroid use is by actually introducing other therapies earlier.
There were multiple presentations at ACR Convergence 2023 evaluating therapies that have the potential to be disease-modifying agents in patients with SLE. For example, we saw results from the long-term extension trial of anifrolumab, which demonstrated reductions over 4 years in disease activity in terms of improvements in SLEDAI-2K (abstract 0597). These data help to solidify the evidence supporting anifrolumab as a potential disease modifier. It meets all the check marks for disease modification at year 1 and through year 4, but we still need longer-term follow-up to show that it has data demonstrating sustained disease modification beyond 5 years.
There was also a lot of excitement at the meeting about the possible use of CAR T-cell therapy and its potential role in disease modification. This included a late-breaking abstract with preliminary data from a phase 1/2 study in patients with severe refractory SLE (abstract L13). Another therapy that was discussed is cenerimod, an S1P1 receptor modulator that has a unique mechanism of action in that it decreases lymphocyte egress from the lymph nodes into the circulation and from the circulation into the tissues. Data presented at ACR Convergence 2023 showed that it decreases disease activity, with the most prominent effect seen in patients with high anti–double-stranded DNA antibody levels and high IFN-1 gene expression signature (abstract 0608).
Overall, the most important take-home message is to make the diagnosis of lupus early and to intervene early. Based on the new Kidney Disease: Improving Global Outcomes (KDIGO) guidelines, you should not wait for a patient’s proteinuria to reach 1 gm before obtaining a biopsy. Consider biopsy with proteinuria as low as 500 mg—and possibly lower if there is clinical suspicion of disease—so that we are able to intervene early and use either low-dose or steroid-free regimens in these patients.
Askanase A. Can current lupus treatments be classified as DMALDs? Session presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Askanase A, D’Cruz D, Kalunian K, et al. Efficacy of cenerimod in patients with high IFN-1 gene expression signature and high anti-dsDNA antibody levels: post-hoc analysis from a phase 2 study [abstract 0608]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Fanouriakis A, Kostopoulou M, Andersen J, et al. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann Rheum Dis. 2023 Oct 12:ard-2023-224762. doi:10.1136/ard-2023-224762
Furie RA, Kalunian K, Morand E, et al. Efficacy of anifrolumab in systemic lupus erythematosus by overall and organ-specific SLEDAI-2K improvements: results from the randomized, placebo-controlled phase 3 long-term extension study [abstract 0597]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Hernández JC, Barba P, Alberich ML, et al. An open-label, multicenter, phase 1/2 study to assess safety, efficacy and cellular kinetics of YTB323, a rapid manufacturing CAR-T cell therapy targeting CD19 on B cells, for severe refractory systemic lupus erythematosus: preliminary results [abstract L13]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO 2023 clinical practice guideline for the management of lupus nephritis. Accessed December 12, 2023. https://kdigo.org/wp-content/uploads/2023/03/KDIGO-2023-Lupus-Nephritis-Guideline_Public-Review_9-Mar-2023.pdf
van Vollenhoven R, Askanase AD, Bomback AS, et al. Conceptual framework for defining disease modification in systemic lupus erythematosus: a call for formal criteria. Lupus Sci Med. 2022;9(1):e000634. doi:10.1136/lupus-2021-000634
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American College of Rheumatology.