Rheumatology
Systemic Lupus Erythematosus
Systemic Lupus Erythematosus: Response to Treatment With Newer Therapies
Overview
As seen at the 2023 Congress of Clinical Rheumatology (CCR) East, the treatment of systemic lupus erythematosus (SLE) continues to evolve, with newer therapies such as anifrolumab, voclosporin, and belimumab now under consideration in various settings.
Following the conference, featured expert Vasileios C. Kyttaris, MD, was interviewed by Christopher Ontiveros, PhD. Clinical perspectives from Dr Kyttaris are presented here.
Vasileios C. Kyttaris, MD
|
|
The 2 main goals in the treatment of SLE are to prevent flares with the use of background medications (eg, hydroxychloroquine) and to treat acute flares with the use of more effective medications (ie, biologics, immunosuppressives, and corticosteroids). We treat flares differently, depending on whether they are arthritis related, nephritis related, or skin related, among other factors. For example, we may use methotrexate for arthritis flares, but we would use mycophenolate or cyclophosphamide for nephritis flares. I think that finding a medication that works for the treatment of all types of flares and is also effective for the prevention of flares would be the holy grail in SLE.
There is a great deal of interest right now in learning how best to incorporate newer treatments for lupus nephritis into our treatment paradigm. We are also interested in determining how newer medications for SLE can help decrease our reliance on corticosteroids, especially the chronic use of corticosteroids for the prevention of flares.
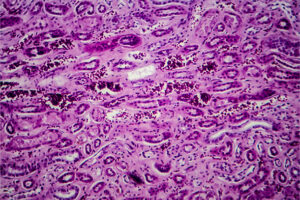
Cyclophosphamide had been a mainstay of treatment for renal SLE in the past, but we are using less and less of it today, and, instead, mycophenolate mofetil has become the standard of care for the treatment of renal SLE. Belimumab and voclosporin can each be combined with standard therapy mycophenolate to treat acute renal flares. In addition, belimumab may also prevent future renal flares, while voclosporin may help limit total corticosteroid use during the treatment of acute lupus nephritis. We still have to determine, however, when belimumab and/or voclosporin should be initiated and how long patients should remain on combination therapy.
In just the last year and a half, we have also added anifrolumab for nonrenal SLE to the treatment armamentarium. Anifrolumab inhibits type I interferon signaling, has been shown to be effective for the treatment of skin disease, and is approved by the US Food and Drug Administration for patients with moderate to severe SLE who are receiving standard therapy. An interesting observation with anifrolumab is that the treatment effect seems to be present quite early. In fact, you can have a clinical effect as early as 8 weeks, and this could have a role in the earlier tapering of corticosteroids. In contrast, with belimumab, you may wait for 6 or 7 months to determine whether it is effective before deciding to move on.
For nonrenal SLE, we are still not using the biologics anifrolumab and belimumab in the first-line setting. For the most part, these agents are used in patients who have failed hydroxychloroquine and at least 1 immunosuppressive agent. Real-world data presented at CCR East by Bell et al suggested that belimumab might have a steroid-sparing effect, but this was not a randomized trial. Other data suggest that anifrolumab may also decrease the cumulative corticosteroid exposure in patients with lupus. I think that both drugs have some evidence that they may help limit the role of steroids, or at least decrease the cumulative corticosteroid exposure, in their respective settings.
Of course, optimizing the use of hydroxychloroquine in SLE also continues to be of interest. Michelle Petri, MD, MPH, touched on the issue of long-term hydroxychloroquine therapy at CCR East. She is a strong advocate for the use of hydroxychloroquine as a background therapy for virtually every patient with lupus, and she presented some data showing that hydroxychloroquine can avert death, prevent thrombosis, and improve the effectiveness of mycophenolate in lupus nephritis.
Nonetheless, hydroxychloroquine is associated with retinal toxicity, especially in patients who have been taking the drug for decades. Because of this, the current recommendation that is backed by the American Academy of Ophthalmology and the American College of Rheumatology is not to use more than 5 mg/kg daily on a chronic basis in order to avoid irreversible visual disturbance or even visual loss. At this point, hydroxychloroquine remains the backbone of therapy for lupus, but that has to be weighed against its potential for toxicity, especially after use for more than a decade.
References
Anders H-J, Loutan J, Bruchfeld A, et al. The management of lupus nephritis as proposed by EULAR/ERA 2019 versus KDIGO 2021. Nephrol Dial Transplant. 2023;38(3):551-561. doi:10.1093/ndt/gfab351
Bell CE, Rubin B, Worley K, et al. Real-world effectiveness of belimumab in patients with systemic lupus erythematosus in the United States. Poster presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Bruce IN, van Vollenhoven RF, Morand EF, et al. Sustained glucocorticoid tapering in the phase 3 trials of anifrolumab: a post hoc analysis of the TULIP-1 and TULIP-2 trials. Rheumatology (Oxford). 2023;62(4):1526-1534. doi:10.1093/rheumatology/keac491
Furie R, Morand EF, Askanase AD, et al. Anifrolumab reduces flare rates in patients with moderate to severe systemic lupus erythematosus. Lupus. 2021;30(8):1254-1263. doi:10.1177/09612033211014267
Furie R, Rovin BH, Houssiau F, et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med. 2020;383(12):1117-1128. doi:10.1056/NEJMoa2001180
Jayne D, Rovin B, Mysler EF, et al. Phase II randomised trial of type I interferon inhibitor anifrolumab in patients with active lupus nephritis. Ann Rheum Dis. 2022;81(4):496-506. doi:10.1136/annrheumdis-2021-221478
Marmor MF, Kellner U, Lai TYY, Melles RB, Mieler WF; American Academy of Ophthalmology. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 revision). Ophthalmology. 2016;123(6):1386-1394. doi:10.1016/j.ophtha.2016.01.058
Mok CC, Teng YKO, Saxena R, Tanaka Y. Treatment of lupus nephritis: consensus, evidence and perspectives. Nat Rev Rheumatol. 2023;19(4):227-238. doi:10.1038/s41584-023-00925-5
Petri M. Comparison of new therapies for SLE. Presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Rovin BH, Solomons N, Pendergraft WF 3rd, et al; AURA-LV Study Group. A randomized, controlled double-blind study comparing the efficacy and safety of dose-ranging voclosporin with placebo in achieving remission in patients with active lupus nephritis. Kidney Int. 2019;95(1):219-231. doi:10.1016/j.kint.2018.08.025
Rovin BH, Teng YKO, Ginzler EM, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial [published correction appears in Lancet. 2021;397(10289):2048]. Lancet. 2021;397(10289):2070-2080. doi:10.1016/S0140-6736(21)00578-X
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the Congress of Clinical Rheumatology.