Rheumatology
Systemic Lupus Erythematosus
Update on Systemic Lupus Erythematosus Biomarkers and Prognostication
As seen at ACR Convergence 2023, researchers continue to work toward improved biomarkers in systemic lupus erythematosus (SLE). Novel biomarkers are being considered, and there is hope that machine learning will help to achieve bold new objectives in SLE.
Following these proceedings, featured expert Vasileios C. Kyttaris, MD, was interviewed by Christopher Ontiveros, PhD. Clinical perspectives from Dr Kyttaris on these proceedings are presented here.
At ACR Convergence 2023, we saw an increasing application of machine learning models to develop SLE biomarkers. Using these models, we are trying to address some of the most complex questions in the field, such as the following: Who is going to develop lupus? This is an important question in the clinic, for example, when you have a patient who has specific serologic findings and vague clinical symptoms, and one is uncertain whether the patient will go on to develop SLE. There is also a desire to diagnose SLE more accurately using a biomarker-based approach that would, perhaps, be less reliant on symptomatology and nonspecific physical examination findings. In addition, one of the most important goals currently is to use biomarkers to predict flares and, more accurately, to monitor disease activity, once again, without so much dependency on symptomatology.
Regarding the different categories of biomarkers, in SLE right now, we are mainly concerned with diagnostic and prognostic biomarkers, as well as biomarkers to help us predict exacerbations and monitor disease. We do not yet have biomarkers that are truly predictive for specific treatments, although there is a lot of work being done in this area. For example, the first US Food and Drug Administration (FDA)–approved biologic for use in lupus (ie, belimumab) targets the cytokine BLyS and is shown to be effective mainly in patients with autoantibody positivity and/or low complement levels. However, these are not exactly predictive biomarkers of effectiveness; rather, the absence of these markers suggests that there is a lower likelihood of response to belimumab.
Two measurements (ie, interferon [IFN]–α levels and the IFN gene expression signature [a measure of exposure and response to IFN-α by peripheral blood cells]) have been analyzed and continue to be studied as potential markers for anti-IFN treatments. These may eventually become useful in predicting response to FDA-approved medications such as anifrolumab, which is an antibody that targets IFN-α receptor 1. At ACR Convergence 2023, Chun Wu et al presented an abstract regarding the usefulness of the IFN signature as a predictive biomarker for response to deucravacitinib, a TYK2 inhibitor that targets the IFN-α pathway, among other targets (abstract 0847). In the phase 2 study of this medication in SLE, although deucravacitinib suppressed the IFN-α gene expression, there was no indication that this marker predicts response, casting doubts about its eventual clinical application.
Whenever I think of diagnostic biomarkers, I tend to think of an objective measure that will help diagnose the disease and also exclude the diagnosis of diseases that may present clinically in a similar fashion. In lupus specifically, the most widely used of the diagnostic biomarkers is the antinuclear antibody, which, according to current thinking, can, when negative, rule out (but not rule in) SLE. Other widely used biomarkers include anti–double-stranded DNA (anti-dsDNA) antibodies, low complement levels, antiphospholipid antibodies, and anti-Smith (anti-Sm) antibodies, all of which vary in sensitivity and specificity for SLE. As has been clearly shown by the new European League Against Rheumatism/American College of Rheumatology SLE criteria, a combination of these biomarkers with clinical manifestations can lead to greater than 90% accuracy in classifying a patient as having SLE. Nevertheless, there is no marker or combination of markers to date that can diagnose SLE by itself without definite clinical manifestations, the way that a positive polymerase chain reaction can diagnose a viral illness, for example.
Now, some of these diagnostic biomarkers are also prognostic. They can suggest to you that the patient is going to develop a more severe disease or specific complications of the disease. For example, anti-Sm antibodies are associated with more severe disease, especially nephritis. The same applies to anti-dsDNA antibodies. Antibodies such as anti-Ro/SSA and anti-La/SSB are associated with sicca and photosensitivity, while anti-RNP antibodies are associated with arthritis and overlap syndromes. So, those are the prognostic biomarkers that may help you determine where the disease is headed, albeit with a modest accuracy.
The aforementioned diagnostic and prognostic biomarkers have not been as helpful in monitoring SLE because they are not very accurate in predicting disease flares. While complement levels tend to decrease, and anti-dsDNA antibody levels tend to rise before and during a disease exacerbation, neither is optimal, as patients may flare without necessarily having abnormal levels, and they can exhibit a rather benign course despite having abnormal levels.
The hope is to come up with more specific biomarkers that can help in the diagnosis, prognosis, and monitoring of SLE. I do not think that we will have a single biomarker that will cover everything, but a combination of different markers may be the answer to better diagnose and monitor the disease. Generally, the studies at this year’s ACR Convergence showed continued efforts in these areas, with some interesting data, but nothing that is necessarily “ready for prime time” without further validation.
Looking at complement activation markers rather than total complement is something that has been of interest for some time now, and we are getting more and more information from larger trials. As the measurement of these markers becomes more standardized and readily available, I think that we are going to potentially be using these more. These include markers such as T-cell bound C4d (TC4d), which was one of the biomarkers of interest in our study that was led by Andrew Concoff, MD (abstract 0576). The idea here is to look beyond measuring the total complement levels (eg, C3 and C4 levels) to estimate complement consumption by measuring complement split products (in this case, TC4d). In this study, beyond TC4d, we measured relevant anti–T-cell IgG and IgM antibodies. In the analysis, we explored the use of a machine-learning model to compare these markers with conventional biomarkers (C3, C4, anti-dsDNA, and anti-Sm antibodies) in differentiating SLE from clinically relevant controls. The results were striking to me, in that we typically think of anti-Sm and anti-dsDNA antibodies as great markers for lupus, but actually, in the cumulative ROC analysis, the TC4d outperformed C3, anti-dsDNA, anti-Sm, and C4. In abstract 2273, we further explored the usefulness of C4d bound to erythrocytes (EC4d) as a way of measuring disease activity objectively, showing that a combination of traditional disease-monitoring markers (C3, C4, anti-dsDNA antibodies) and novel biomarkers (EC4d and PC4d) predicts clinical activity with high accuracy. The focus of these studies was diagnosis and monitoring of the disease, but, ultimately, we may be able to use additional markers such as these to better predict flares.
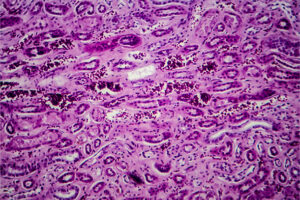
Another interesting approach seeks to improve the estimate of intrarenal inflammation by looking at not only proteinuria but also cells or soluble mediators that may leak in the urine during high disease activity but may not be present at the same levels if the kidney disease is quiescent. One report from ACR Convergence 2023 that caught my attention in this area was by Andrea Fava, MD, and colleagues (abstract 0850), who looked at different combinations of biomarkers in the urine, notably including interleukin 16 (IL-16), a rather obscure cytokine in the sense that we were not used to thinking of it as a major mediator of disease activity in lupus. These investigators showed that the urine levels of this cytokine can predict kidney failure even more accurately than the urinary protein to creatinine ratio. Moreover, the same group showed that IL-16 is released by multiple immune cell types in the kidneys of patients with lupus nephritis and hypothesized that it may promote and amplify lupus nephritis (abstract 0915).
Ultimately, we will probably want to move toward a combination of biomarkers of serological activity or systemic inflammation, along with measurements in the urine of intrarenal inflammation, because, given the extreme heterogeneity of SLE presentation and fluctuations of disease activity, we might not be able to rely on using just serum or urinary markers alone in all patients.
Aringer M, Costenbader KH, Daikh DI, et al. 2019 EULAR/ACR classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71(9):1400-1412. doi:10.1002/art.40930
Carter LM, Wigston Z, Laws P, Vital EM. Rapid efficacy of anifrolumab across multiple subtypes of recalcitrant cutaneous lupus erythematosus parallels changes in discrete subsets of blood transcriptomic and cellular biomarkers. Br J Dermatol. 2023;189(2):210-218. doi:10.1093/bjd/ljad089
Celia AI, Yang X, Minsky H, et al. IL-16+ is abundantly expressed by kidney-infiltrating myeloid and lymphoid cells in lupus nephritis: a spatially resolved multiplexed approach [abstract 0915]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Concoff A, Kyttaris V, Sandhu V, et al. Enhancing systemic lupus erythematosus diagnosis: comparative performance characteristics of TC4d and anti-T-cell antibodies with conventional biomarkers [abstract 0576]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Fava A, Atta MG, Monroy-Trujillo J, et al. Persistence of urinary biomarkers of intrarenal inflammation precedes loss of kidney function in lupus nephritis [abstract 0850]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Hubbard EL, Pisetsky DS, Lipsky PE. Anti-RNP antibodies are associated with the interferon gene signature but not decreased complement levels in SLE. Ann Rheum Dis. 2022;81(5):632-643. doi:10.1136/annrheumdis-2021-221662
Kingsmore KM, Puglisi CE, Grammer AC, Lipsky PE. An introduction to machine learning and analysis of its use in rheumatic diseases. Nat Rev Rheumatol. 2021;17(12):710-730. doi:10.1038/s41584-021-00708-w
Kyttaris V, O’Malley T, Casaburi G, Kumar S, Concoff A. Predicting SLE disease activity with blood biomarkers: a step towards precision medicine [abstract 2273]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
Nawata A, Nakayamada S, Hisano S, et al. Differential expression of IFN-α, IL-12 and BAFF on renal immune cells and its relevance to disease activity and treatment responsiveness in patients with proliferative lupus nephritis. Lupus Sci Med. 2023;10(2):e000962. doi:10.1136/lupus-2023-000962
Sarkar MK, Hile GA, Tsoi LC, et al. Photosensitivity and type I IFN responses in cutaneous lupus are driven by epidermal-derived interferon kappa. Ann Rheum Dis. 2018;77(11):1653-1664. doi:10.1136/annrheumdis-2018-21319
Wu C, Hu Y, Crow MK, et al. Development of an IFN 5-gene signature score to identify IFN-high and IFN-low subsets and as a pharmacodynamic biomarker for deucravacitinib treatment in a phase 2 trial in patients with systemic lupus erythematosus [abstract 0847]. Abstract presented at: ACR Convergence 2023; November 10-15, 2023; San Diego, CA.
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American College of Rheumatology.