Oncology
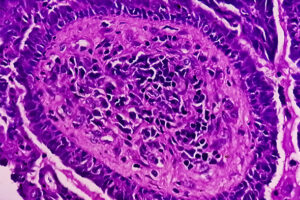
Endometrial Cancer
Endometrial Cancer and Obesity
The rising tide of overweight and obesity is contributing to the increased incidence of endometrial cancer worldwide. Presentations earlier in life (during the childbearing years) and morbid obesity–associated surgical risks are 2 related concerns.
Obesity is a very well-known—and probably the strongest—risk factor for developing endometrial cancer. In an analysis of 26 studies by the American Institute for Cancer Research, there was a 50% increased risk of developing endometrial cancer for every increase of 5 body mass index units. So, as the obesity rate increases, the incidence of endometrial cancer goes up, including among younger women.
The median age for a diagnosis of endometrial cancer is approximately 60 years, and it is less common under the age of 45 years; however, there is still a significant percentage of women who are premenopausal at diagnosis. In fact, I have even seen patients who were diagnosed before the age of 30, and it is likely that obesity is contributing to the numbers that we are seeing. Many of these younger women have treatable disease and can be cured, but this is at a point in life when there can be concerns about fertility. Thus, the net effect is also to increase the population of women who may be interested in fertility-preserving treatment.
Not only does obesity increase the risk of endometrial cancer but it can also negatively impact surgical options and can complicate postoperative recovery. Treating patients who are morbidly obese becomes more challenging. For example, they may no longer be candidates for surgery if their body mass index is too high. Most endometrial cancers are treated surgically, usually with a minimally invasive approach. For these procedures, we use the Trendelenburg position, which is not always well tolerated in the setting of morbid obesity. So, a person’s weight can adversely impact our ability to use a minimally invasive approach and is certainly something that we discuss with the patient. Finally, obesity also increases a patient’s risk of complications from surgery, including wound breakdown.
Although we cannot change a patient’s diagnosis of endometrial cancer once it occurs, we can still talk to patients about the benefits of lifestyle changes and encourage them in their attempts to maintain a healthy weight.
Byun D, Hong S, Ryu S, et al. Early-life body mass index and risks of breast, endometrial, and ovarian cancers: a dose-response meta-analysis of prospective studies. Br J Cancer. 2022;126(4):664-672. doi:10.1038/s41416-021-01625-1
Cancer stat facts: uterine cancer. National Cancer Institute Surveillance, Epidemiology, and End Results Program. Accessed October 26, 2023. https://seer.cancer.gov/statfacts/html/corp.html
Committee on Gynecologic Practice. Committee opinion no. 619: gynecologic surgery in the obese woman. Obstet Gynecol. 2015;125(1):274-278. doi:10.1097/01.AOG.0000459870.06491.71
Derbyshire AE, MacKintosh ML, Pritchard CM, et al. Women’s risk perceptions and willingness to engage in risk-reducing interventions for the prevention of obesity-related endometrial cancer. Int J Womens Health. 2022;14:57-66. doi:10.2147/IJWH.S326417
Guo F, Levine L, Berenson A. Trends in the incidence of endometrial cancer among young women in the United States, 2001 to 2017 [abstract 5578]. Abstract presented at: 2021 American Society of Clinical Oncology Annual Meeting; June 4-8, 2021.
Harvey SV, Wentzensen N, Bertrand K, et al. Associations of life course obesity with endometrial cancer in the Epidemiology of Endometrial Cancer Consortium (E2C2). Int J Epidemiol. 2023;52(4):1086-1099. doi:10.1093/ije/dyad046
Kiesel L, Eichbaum C, Baumeier A, Eichbaum M. Obesity epidemic—the underestimated risk of endometrial cancer. Cancers (Basel). 2020;12(12):3860. doi:10.3390/cancers12123860
Leone Roberti Maggiore U, Khamisy-Farah R, Bragazzi NL, et al. Fertility-sparing treatment of patients with endometrial cancer: a review of the literature. J Clin Med. 2021;10(20):4784. doi:10.3390/jcm10204784
Li M, Guo T, Cui R, Feng Y, Bai H, Zhang Z. Weight control is vital for patients with early-stage endometrial cancer or complex atypical hyperplasia who have received progestin therapy to spare fertility: a systematic review and meta-analysis. Cancer Manag Res. 2019;11:4005-4021. doi:10.2147/CMAR.S194607
Mahdi H, Jernigan AM, Aljebori Q, Lockhart D, Moslemi-Kebria M. The impact of obesity on the 30-day morbidity and mortality after surgery for endometrial cancer. J Minim Invasive Gynecol. 2015;22(1):94-102. doi:10.1016/j.jmig.2014.07.014
Onstad MA, Schmandt RE, Lu KH. Addressing the role of obesity in endometrial cancer risk, prevention, and treatment. J Clin Oncol. 2016;34(35):4225-4230. doi:10.1200/JCO.2016.69.4638
Raglan O, Kalliala I, Markozannes G, et al. Risk factors for endometrial cancer: an umbrella review of the literature. Int J Cancer. 2019;145(7):1719-1730. doi:10.1002/ijc.31961
World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project 2013. Diet, nutrition, physical activity and endometrial cancer. Revised 2018. Accessed October 31, 2023. https://www.wcrf.org/wp-content/uploads/2021/02/Endometrial-cancer-report.pdf