Rheumatology
Systemic Lupus Erythematosus
Improving Long-term Outcomes in Systemic Lupus Erythematosus: Trends and Contributors
Overview
Treatment goals in systemic lupus erythematosus (SLE) include achieving long-term patient survival, preventing flares and organ damage, and safeguarding health-related quality of life. The management of disease-related and treatment-related comorbidities, especially infections and atherosclerosis, is of great importance in the achievement of these goals.
What are the drivers of long-term outcomes in SLE, and what factors account for the observed improvements?
George C. Tsokos, MD
|
|
“Patients with SLE have a risk from cardiovascular complications and a risk from kidney disease, and such risks are not simply additive, as one can worsen the other.”
The management of SLE has improved over the last 40 years, with an improvement in long-term outcomes, which could be partly attributed to the treatment of comorbidities and the prevention of complications. Certainly, tacrolimus and mycophenolate mofetil (MMF) were influential; however, so was learning more about the cardiovascular complications, managing them early, and treating diabetes and hypertension aggressively in patients with lupus. Perhaps more importantly, the approach to infections, including prompt identification and treatment in patients with lupus, has had a significant impact.
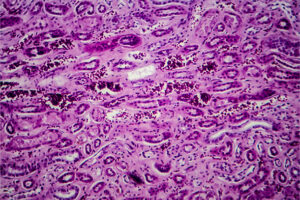
Patients with SLE have a risk from cardiovascular complications and a risk from kidney disease, and such risks are not simply additive, as one can worsen the other. If I were to develop a master plan to teach the next generation of clinicians about managing lupus, I would reinforce the importance of the early identification of comorbidities, since these complications have an undesirable and oftentimes synergistic effect on patient outcomes.
Nephrologists play an important role because they tend to have an aggressively nephroprotective attitude, whether it is treating hypertension to target, hypercholesterolemia, proteinuria, or infection (eg, subclinical, smoldering urinary tract infections), and I believe that these efforts translate to better outcomes for patients with SLE.
We also have a better understanding of neuropsychiatric comorbidity, especially depression and how it impacts a patient’s life. Moreover, it is important to recognize depression early, even in mild forms and in younger patients, because it can affect the long-term prognosis of patients with SLE. It is not all in their heads; there is a biologic substrate, and if we can help them in this way, there should also be a beneficial impact on their lives and on the management of their SLE.
Joan T. Merrill, MD
|
|
". . . SLE itself and its management are important factors in long-term outcomes.”
Studies have demonstrated that patients with more disease activity have worse outcomes. A number of cohort studies, mostly conducted by members of the Systemic Lupus Erythematosus International Collaborative Clinics but also by some others, have demonstrated this repeatedly. Moreover, work by Morand and colleagues in Australia examined the opposite question: If you can get to a certain degree of low disease activity, does that improve outcomes? And it does. So, I think that the writing is on the wall, and that SLE itself and its management are important factors in long-term outcomes.
It is clear that patients with SLE who have better cardiovascular health will fare better, as will those who benefit from all of the other kinds of improved care that we have these days. However, not all patients with SLE really do have better cardiovascular health care these days. Patients with lupus, especially those who are minorities, have limited access to quality medical care. This could be due to a lack of good health insurance, limiting their access to specialists. And in that setting, primary care suffers as well.
As Dr Tsokos alluded to, there may be a mind and body connection between lupus and psychiatric comorbidity. Lupus is an immune disorder, not a psychiatric disease, but patients with depression may be less likely to seek out treatment for their SLE. Additionally, a healthy person who contracts a virus may be sick for 5 days, for example, but a patient with lupus might continue to be impacted for a year.
Bevra H. Hahn, MD
|
|
“A better understanding of the importance of preventing comorbidities and of incremental improvements in SLE treatment have both been significant in improving survival in patients with SLE.”
A better understanding of the importance of preventing comorbidities and of incremental improvements in SLE treatment have both been significant in improving survival in patients with SLE. The introductions of cyclophosphamide and MMF were major advances. Belimumab was another helpful addition to the SLE treatment armamentarium, and more recent data suggest that it may protect the kidneys from long-term damage. A 2-year, randomized, placebo-controlled study demonstrated that the risk of a renal-related event or death was lower among patients who received belimumab than among those who received placebo. A renal‐related event was defined as any of the following: end‐stage kidney disease, a doubling of the serum creatinine level from the baseline level, increased proteinuria, impaired kidney function, or kidney disease–related treatment failure. Additionally, 2 new therapies have recently been approved by the US Food and Drug Administration for SLE. Voclosporin, an oral medication, added to MMF plus low-dose steroids, produces a more rapid improvement in lupus nephritis than MMF plus steroids alone, and a higher proportion of patients have an excellent response. Voclosporin is related to tacrolimus and cyclosporine—all inhibit T-lymphocyte function, and voclosporin also protects some kidney cells from damage. Anifrolumab is an antibody that interferes with cell responses to type I interferon, a cytokine that is elevated in many patients with SLE. Anifrolumab is effective in SLE without nephritis, particularly in those with lupus rashes. Just how useful these exciting new medications are for patients with SLE will be clear over the next year or 2.
We have also made several major strides in preventing comorbidities in patients with SLE. One of the most significant advances has been the international campaign to reduce steroid use. Reducing prednisone doses to 7.5 mg or less minimizes the possibility of steroid-induced damage. And, with the availability of steroid-sparing treatments and combinations, we can achieve and maintain lower steroid doses in some patients. There has also been an increased emphasis on aggressively treating hyperlipidemia, hypertension, and osteoporosis in patients with SLE. And, clearly, these comorbidities may be impacted by steroid use. Finally, infection prevention is a major focus in SLE in view of both the disease and immunosuppressive therapy. The availability of the recombinant (ie, not live-attenuated) herpes zoster vaccine has been an advancement for patients with SLE, as herpes zoster is common, particularly in patients treated with anifrolumab.
While we are pleased with the improved survival and other long-term outcomes in patients with SLE, there is still the need to improve end-stage renal disease and to reduce renal transplant, which we hope will be possible with the availability of new therapeutic approaches.
References
Arnaud L, Tektonidou MG. Long-term outcomes in systemic lupus erythematosus: trends over time and major contributors. Rheumatology (Oxford). 2020;59(suppl 5):v29-v38. doi:10.1093/rheumatology/keaa382
Chatham WW, Furie R, Saxena A, et al. Long-term safety and efficacy of anifrolumab in adults with systemic lupus erythematosus: results of a phase II open-label extension study [published correction appears in Arthritis Rheumatol. 2021;73(8):1570]. Arthritis Rheumatol. 2021;73(5):816-825. doi:10.1002/art.41598
Furie R, Rovin BH, Houssiau F, et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med. 2020;383(12):1117-1128. doi:10.1056/NEJMoa2001180
Gatto M, Saccon F, Zen M, et al. Early disease and low baseline damage as predictors of response to belimumab in patients with systemic lupus erythematosus in a real-life setting. Arthritis Rheumatol. 2020;72(8):1314-1324. doi:10.1002/art.41253
Legge A, Kirkland S, Rockwood K, et al. Evaluating the properties of a frailty index and its association with mortality risk among patients with systemic lupus erythematosus. Arthritis Rheumatol. 2019;71(8):1297-1307. doi:10.1002/art.40859
Maria NI, Davidson A. Protecting the kidney in systemic lupus erythematosus: from diagnosis to therapy. Nat Rev Rheumatol. 2020;16(5):255-267. doi:10.1038/s41584-020-0401-9
Mathian A, Pha M, Haroche J, et al. Withdrawal of low-dose prednisone in SLE patients with a clinically quiescent disease for more than 1 year: a randomised clinical trial. Ann Rheum Dis. 2020;79(3):339-346. doi:10.1136/annrheumdis-2019-216303
Morand EF, Furie R, Tanaka Y, et al; TULIP-2 Trial Investigators. Trial of anifrolumab in active systemic lupus erythematosus. N Engl J Med. 2020;382(3):211-221. doi:10.1056/NEJMoa1912196
Morand EF, Mosca M. Treat to target, remission and low disease activity in SLE. Best Pract Res Clin Rheumatol. 2017;31(3):342-350. doi:10.1016/j.berh.2017.09.009
Moustafa AT, Moazzami M, Engel L, et al. Prevalence and metric of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. Semin Arthritis Rheum. 2020;50(1):84-94. doi:10.1016/j.semarthrit.2019.06.017
Munguia-Realpozo P, Mendoza-Pinto C, Sierra Benito C, et al. Systemic lupus erythematosus and hypertension. Autoimmun Rev. 2019;18(10):102371. doi:10.1016/j.autrev.2019.102371
Rovin BH, Teng YKO, Ginzler EM, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial [published correction appears in Lancet. 2021;397(10289):2048]. Lancet. 2021;397(10289):2070-2080. doi:10.1016/S0140-6736(21)00578-X
Yu H-H, Chen P-C, Yang Y-H, et al. Statin reduces mortality and morbidity in systemic lupus erythematosus patients with hyperlipidemia: a nationwide population-based cohort study. Atherosclerosis. 2015;243(1):11-18. doi:10.1016/j.atherosclerosis.2015.08.030