Rheumatology
Systemic Lupus Erythematosus
Low-Dose Interleukin 2 and Its Potential in Systemic Lupus Erythematosus
Overview
Low-dose interleukin-2 (IL-2) therapy continues to be studied as a potential approach for systemic lupus erythematosus (SLE), where it may restore regulatory T-cell (Treg) homeostasis and prevent global immunosuppression. Preclinical and early clinical data have been encouraging; however, additional investigation is required.
Expert Commentary
George C. Tsokos, MD
|
|
“Low-dose IL-2 is an investigational treatment approach in SLE that has shown promise in preclinical and early clinical studies.”
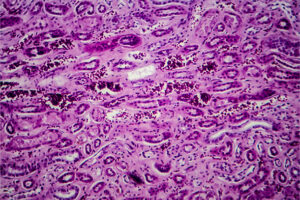
As a result of my career-long research on the impact of low IL-2 production in SLE, I have been an advocate for the further exploration and clinical development of low-dose IL-2 as a potential treatment strategy in this patient population. Our group generated data demonstrating the importance of IL-2 in mice with lupus, which piqued the interest of other investigators in the field. We had seen that IL-2–deficient mice develop severe autoimmunity marked by reduced Treg numbers and the systemic expansion of pathogenic T-cell effectors, which suggested that IL-2 is crucial for the maintenance of T-cell–mediated self-tolerance. Our data also suggested that the administration of IL-2 to lupus-prone mice protects against end-organ damage and suppresses inflammation by dually limiting IL-17–producing CD3+CD4-CD8- (double-negative) T cells and expanding Treg.
Low-dose IL-2 is an investigational treatment approach in SLE that has shown promise in preclinical and early clinical studies. Since IL-2 is upstream from several pathways, the administration of low-dose IL-2 allows for the following to occur: (1) the correction of Tregs; (2) the suppression of T helper 17 cell production; (3) the suppression of CD41+ T cells and T follicular helper cells; and (4) the enhancement of cytotoxic responses, which is needed in patients with SLE. In fact, the lack of IL-2 production by the CD41+ T cells of patients with SLE may account for the loss of CD25 expression in Tregs, which could be selectively reversed by stimulation with low doses of IL-2.
While there is plenty of reason for optimism based on preclinical data, the clinical data have been relatively limited thus far. There is a placebo-controlled, single-center trial conducted by He et al in which 60 patients with active SLE had rapid and significant disease improvement at week 24 with low-dose IL-2 therapy compared with placebo (Systemic Lupus Erythematosus Responder Index 4 response, 66% vs 37%). Total cumulative corticosteroid doses were also reduced more during treatment with low-dose IL-2 than with placebo. With minimal side effects and the opportunity to limit the total cumulative corticosteroid dose, I am optimistic that low-dose IL-2 will become a beneficial supplement in SLE management, but further study is required.
References
He J, Zhang R, Shao M, et al. Efficacy and safety of low-dose IL-2 in the treatment of systemic lupus erythematosus: a randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. 2020;79(1):141-149. doi:10.1136/annrheumdis-2019-215396
Humrich JY, Riemekasten G. Low-dose interleukin-2 therapy for the treatment of systemic lupus erythematosus. Curr Opin Rheumatol. 2019;31(2):208-212. doi:10.1097/BOR.0000000000000575
Katsuyama E, Suarez-Fueyo A, Bradley SJ, et al. The CD38/NAD/SIRTUIN1/EZH2 axis mitigates cytotoxic CD8 T cell function and identifies patients with SLE prone to infections. Cell Rep. 2020;30(1):112-123.e4. doi:10.1016/j.celrep.2019.12.014
Li H, Tsokos MG, Bickerton S, et al. Precision DNA demethylation ameliorates disease in lupus-prone mice. JCI Insight. 2018;3(16):e120880. doi:10.1172/jci.insight.120880
Mizui M, Koga T, Lieberman LA, et al. IL-2 protects lupus-prone mice from multiple end-organ damage by limiting CD4-CD8-IL-17-producing T cells. J Immunol. 2014;193(5):2168-2177. doi:10.4049/jimmunol.1400977
Tahvildari M, Dana R. Low-dose IL-2 therapy in transplantation, autoimmunity, and inflammatory diseases. J Immunol. 2019;203(11):2749-2755. doi:10.4049/jimmunol.1900733