Rheumatology
Systemic Lupus Erythematosus
The Treatment Target in Newly Diagnosed Systemic Lupus Erythematosus: Preventing Early Damage
Overview
Treat-to-target strategies in systemic lupus erythematosus (SLE) involve setting the treatment target to complete remission or to low disease activity when complete remission is not possible. Early responses are sought, owing to their association with better outcomes.
What are your thoughts on the treat-to-target paradigm? Is there an early window of opportunity in SLE?
Bevra H. Hahn, MD
|
|
“ . . . yes, achieving a good, early response is the goal, but there are several caveats. First, achieving that goal is only partially dependent on the treatment.”
We have known for a long time that good, early responses are associated with better long-term outcomes in SLE, and this is true in many diseases. So, yes, achieving a good, early response is the goal, but there are several caveats. First, achieving that goal is only partially dependent on the treatment. In some cases, you can do everything that all of the guidelines recommend, but the patient still does not respond. So, treat to target is a good idea, but it is not always easy. Additionally, there is a balance involved (ie, if an early responder dies from an infection from the immunosuppression, it does not matter that they were an early responder).
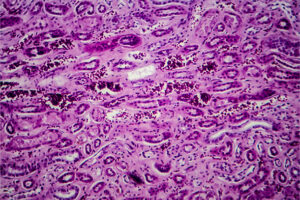
Regarding lupus nephritis, the 2019 update from the European League Against Rheumatism (EULAR) noted that patients with an early significant reduction in proteinuria (defined as ≤1 g/day at 6 months or ≤0.8 g/day at 12 months) are more likely to have favorable long-term renal outcomes. There are also other benchmarks along the way. You can look at 3 months and 6 months and see whether you are getting closer to your target. EULAR defines a partial remission in lupus nephritis as a 50% or greater reduction in proteinuria to subnephrotic levels and serum creatinine within 10% from baseline by 6 to 12 months. If you observe a 20% decrease in proteinuria by 3 months and a 50% decrease by 6 months, and then you get down to 0.7 g per day or less, you will be in good shape. As you monitor along the way, if the patient tolerates it, you can do add-ons to achieve that goal; but patient tolerability is important, so it is good that we have several choices in therapy. It is concerning when a patient does not respond within the first 12 months. They may respond to something else, but you have lost a fair number of glomeruli by the time you get to that point.
Short of complete remission, different definitions of low disease activity have been proposed. The Asia Pacific Lupus Collaboration undertook a series of studies to define and validate the Lupus Low Disease Activity State (LLDAS), which has been independently associated with less damage accrual. The LLDAS uses a more lenient definition that allows for some disease activity, including Systemic Lupus Erythematosus Disease Activity Index 2000 scores of 4 or less. Even with this generous definition, however, the LLDAS was attained in just under half of all visits in a study by Golder et al.
Joan T. Merrill, MD
|
|
“ . . . I believe that the message should not be that we can get to a low disease activity state and stop there, but, instead, that we at least get to low disease activity and then do our best to help our patients achieve total remission.”
Regarding the treat-to-target approach in SLE, one of the best aspects of these targets is to remind us that we should not be complacent about grumbling disease. Morand and colleagues have advanced 2 main ideas: that we would love to get all patients with SLE into remission and that, short of remission, there may be a “sweet spot” that is more feasible yet still influences a patient’s prognosis and prevents damage. And the data suggest that spending more time in a state of low disease activity does improve outcomes.
However, I believe that the message should not be that we can get to a low disease activity state and stop there, but, instead, that we at least get to low disease activity and then do our best to help our patients achieve total remission. We must keep trying. If I were to treat my daughter for SLE, for instance, I would be happy if she attained low disease activity, but I would continue to search for ways to make her better. And, of course, making people better will always be our goal.
Ultimately, I think that this idea of a sweet spot is important in more ways than one. For example, there are a lot of lupus trials showing that the middle dose is working but the high dose is not. When you have seen 8 or 9 studies with these outcomes, you start wondering whether we have missed the sweet spot (ie, is more always necessarily more?).
George C. Tsokos, MD
|
|
“ . . . the concept of treat to target coexists—and is at times at odds—with that of disease heterogeneity in SLE. . . . we owe it to our patients to treat to target. . . . However, regardless of how effectively we treat our patients, there may still be some patients who will not respond to treatment due to the heterogeneity of the disease.”
With respect to what Drs Hahn and Merrill have discussed, I believe that the concept of treat to target coexists—and is at times at odds—with that of disease heterogeneity in SLE. That is, not all lupus nephritis is the same, not all lupus will present the same, and it is true that there are people with lupus nephritis who will not respond, no matter what you do.
But we all want to be effective clinicians and actively manage the problems that the patient is experiencing. Therefore, we owe it to our patients to treat to target. I do believe in early treatment; the data are good in SLE like they are in rheumatoid arthritis. We need to address every issue that can compromise the long-term function of the organ. By doing this, we can hopefully minimize the accrual of organ damage. However, regardless of how effectively we treat our patients, there may still be some patients who will not respond to treatment due to the heterogeneity of the disease.
References
Aringer M, Leuchten N, Schneider M. Treat to target in systemic lupus erythematosus. Rheum Dis Clin North Am. 2019;45(4):537-548. doi:10.1016/j.rdc.2019.07.004
Dall’Era M, Cisternas MG, Smilek DE, et al. Predictors of long-term renal outcome in lupus nephritis trials: lessons learned from the Euro-Lupus Nephritis cohort. Arthritis Rheumatol. 2015;67(5):1305-1313. doi:10.1002/art.39026
Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78(6):736-745. doi:10.1136/annrheumdis-2019-215089
Floris A, Piga M, Perra D, et al. Treatment target in newly diagnosed systemic lupus erythematosus: the association of lupus low disease activity state and remission with lower accrual of early damage. Arthritis Care Res (Hoboken). 2020;72(12):1794-1799. doi:10.1002/acr.24086
Franklyn K, Lau CS, Navarra SV, et al; Asia-Pacific Lupus Collaboration. Definition and initial validation of a Lupus Low Disease Activity State (LLDAS). Ann Rheum Dis. 2016;75(9):1615-1621. doi:10.1136/annrheumdis-2015-207726
Golder V, Kandane-Rathnayake R, Huq M, et al. Lupus low disease activity state as a treatment endpoint for systemic lupus erythematosus: a prospective validation study. Lancet Rheumatol. 2019;1(2):E95-E102. doi:https://doi.org/10.1016/S2665-9913(19)30037-2
Golder V, Tsang-A-Sjoe MWP. Treatment targets in SLE: remission and low disease activity state. Rheumatology (Oxford). 2020;59(suppl 5):v19-v28. doi:10.1093/rheumatology/keaa420
Morand EF, Mosca M. Treat to target, remission and low disease activity in SLE. Best Pract Res Clin Rheumatol. 2017;31(3):342-350. doi:10.1016/j.berh.2017.09.009
Morand EF, Trasieva T, Berglind A, Illei GG, Tummala R. Lupus Low Disease Activity State (LLDAS) attainment discriminates responders in a systemic lupus erythematosus trial: post-hoc analysis of the phase IIb MUSE trial of anifrolumab. Ann Rheum Dis. 2018;77(5):706-713. doi:10.1136/annrheumdis-2017-212504
van Vollenhoven RF, Mosca M, Bertsias G, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis. 2014;73(6):958-967. doi:10.1136/annrheumdis-2013-205139