Oncology
Mantle Cell Lymphoma
Chimeric Antigen Receptor T-Cell Therapy for Mantle Cell Lymphoma
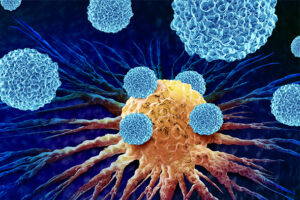
Chimeric antigen receptor (CAR) T-cell therapy involves a patient’s T cells being extracted from their blood and modified to recognize and attack their cancer cells. This therapy has been tested extensively in patients with relapsed and refractory mantle cell lymphoma (MCL) who have few other treatment options. Updated results were recently published from a pivotal phase 2 trial evaluating the CAR T-cell therapy brexucabtagene autoleucel.
Results of the phase 2 ZUMA-2 trial showed that the CAR T-cell therapy brexucabtagene autoleucel can have a high response rate for many patients with MCL, even those who have been very heavily pretreated. CAR T-cell therapy does have toxicities, including pancytopenia, infections, cytokine release syndrome, neurologic toxicity, and cardiovascular toxicity. Nonetheless, I think that patients who were enrolled in ZUMA-2 really did not have many good options, and the results were amazing. Even the long-term follow-up showed fairly good progression-free and overall survival.
More recently, a US lymphoma consortium with real-world data showed that results from undergoing treatment with CAR T-cell therapy really hold up over time, including in patients who would not have met the eligibility criteria of the ZUMA-2 study. So, I think that CAR T-cell therapy is an excellent option for certain patient populations and one that will probably be used more and more as people gain additional experience with it.
In my view, an ideal candidate with MCL for CAR T-cell therapy is a patient with standard risk who has gone through typical upfront therapy, a second-line BTK inhibitor, and now needs third-line treatment. I would say that patients with high-risk features, such as TP53 abnormalities, or those who are heavily pretreated probably do not benefit as much from CAR T-cell therapy as other patients, but that is true with any treatment for MCL.
There are limiting factors, even when CAR T-cell therapy is indicated. For patients with more aggressive disease, it is definitely difficult to obtain insurance approval. Typically, submitting for insurance approval is a 2-step process. First, you need to complete the testing that is required by the insurance company, which includes an echocardiogram, infectious disease testing, some basic blood work, and a social work consult. The second step is negotiating a single-case agreement for each patient with private insurance. The entire process can take more than 4 weeks for some patients, and it is very labor intensive.
Given this delay, there is often a need for a bridging therapy to control the patient’s MCL until CAR T-cell therapy can be administered. This therapy does not need to produce a big response, but, certainly, if the patient is symptomatic or has extensive disease, they need bridging therapy. The choice of a bridging therapy depends on the patient’s prior treatments. We also try to avoid using bendamustine, as it has been associated with worse outcomes for CAR T cells.
There are other limitations to therapy. Patients with the blastoid variant or highly mutated MCL that is too aggressive may not be able to wait for CAR T-cell treatment, even with bridging therapy. And, although there are fewer side effects with CAR T-cell therapy than with autotransplant if nothing goes wrong, you cannot predict tolerability. So, if patients have underlying neurologic issues, a very poor performance status, or cardiac issues, they might not be candidates for CAR T-cell therapy. Pirtobrutinib is a well-tolerated alternative with good outcomes for these patients.
I want to emphasize that I think that a lot of patients with MCL who could potentially benefit from CAR T-cell therapy are not being referred because some referring physicians feel that their patients are not candidates. However, in many patients, CAR T-cell therapy is better tolerated than an autologous stem cell transplant, so I would like to see an increased number of referrals for patients who are potentially eligible.
Amini L, Silbert SK, Maude SL, et al. Preparing for CAR T cell therapy: patient selection, bridging therapies, and lymphodepletion. Nat Rev Clin Oncol. 2022;19(5):342-355. doi:10.1038/s41571-022-00607-3
Mahmood SS, Riedell PA, Feldman S, et al. Biomarkers and cardiovascular outcomes in chimeric antigen receptor T-cell therapy recipients. Eur Heart J. 2023;44(22):2029-2042. doi:10.1093/eurheartj/ehad117
Wang M, Munoz J, Goy A, et al. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2020;382(14):1331-1342. doi:10.1056/NEJMoa1914347
Wang M, Munoz J, Goy A, et al. Three-year follow-up of KTE-X19 in patients with relapsed/refractory mantle cell lymphoma, including high-risk subgroups, in the ZUMA-2 study. J Clin Oncol. 2023;41(3):555-567. doi:10.1200/JCO.21.02370
Wang Y, Jain P, Locke FL, et al. Brexucabtagene autoleucel for relapsed or refractory mantle cell lymphoma in standard-of-care practice: results from the US Lymphoma CAR T Consortium. J Clin Oncol. 2023;41(14):2594-2606. doi:10.1200/JCO.22.01797