Oncology
Mantle Cell Lymphoma
Personalizing the Approach to Treatment-Naive Mantle Cell Lymphoma
Classically, personalizing the initial treatment of mantle cell lymphoma (MCL) has involved considering factors such as patient age and comorbidities to guide decisions about therapeutic intensity. Today, there is also a desire to be able to offer patients a more tailored approach in view of factors such as the TP53 mutational status.
Historically, one level of treatment personalization has been very basic. Older, more frail patients receive treatments that are not so intense while younger, healthier patients receive other treatments that are more intense, and, of course, patient preferences also come into play. But I think that there is room to refine that, and we are looking for additional opportunities. For example, patients with TP53-mutated disease should definitely receive an alternative treatment, since we know that their outcomes with chemotherapy are poor. This might involve using targeted therapies and maybe moving chimeric antigen receptor (CAR) T-cell therapy to earlier in their treatment. We do not have a large amount of data telling us how effective these nonchemotherapy approaches will be up front in TP53-mutated MCL, but I think that these data will be generated in the next couple of years. To put it another way, for the less than 10% of patients who have TP53-mutated disease up front, we know what does not work (ie, chemotherapy), but we do not yet know what does work. So far, we have largely abandoned what does not work and are trying other things.
For the cases of MCL that are much more proliferative, even if these patients do not have a TP53 mutation, they should potentially be handled a bit differently from the cases of MCL with a slow growth rate. I think that there are opportunities to personalize treatment for these patients and to learn which groups of patients need high-dose cytarabine or stem cell transplantation. We need more studies and more data, and that will not be simple because MCL is an uncommon lymphoma.
The TRIANGLE study may potentially turn the whole field on its head. In TRIANGLE, the small-molecule kinase inhibitor ibrutinib was added to the standard chemotherapy regimen, with or without autologous stem cell transplantation. Results were presented at the 64th American Society of Hematology Annual Meeting and Exposition last year. TRIANGLE is not published yet, but the data suggest that adding a BTK inhibitor to frontline therapy may mean that you do not have to put the patient through a stem cell transplant. However, we do not have regulatory approval from the US Food and Drug Administration for BTK inhibitors in the frontline setting, and the BTK inhibitor that was used in this trial (ie, ibrutinib) has been withdrawn from the US market. As a result, we have really interesting data but not much ability to act on it right now. So, it has been a bit of an awkward year in MCL.
When personalizing care, many factors are taken into consideration, including patient age, their overall health, and whether their mantle cells have a TP53 abnormality. Testing for a TP53 abnormality should be performed in every case. You also have to consider the patient’s preferences. Do they want to undergo aggressive treatment? A lot of younger patients are still very interested in receiving aggressive treatment. There are also clinical trials that are available, and participation in a trial is something that we offer patients because we do not know the best treatment. So, personalizing care involves a very long discussion with each individual patient.
MCL is quite indolent in some patients, so, for individuals with MCL, there is not a rush to choose a treatment. You can talk with these patients about their options, and they can come back at a later time. Rarely, MCL can be very aggressive, presenting either at diagnosis, which is rare, or after a relapse, and you do not have a lot of time with these patients to make decisions. Nonetheless, the majority of individuals with MCL do not have to make an immediate decision regarding treatment. You can discuss options with the patient for a period of time.
The EA4151 trial is examining the value of minimal residual disease–guided decision making. After patients undergo induction therapy, those who are minimal residual disease negative are randomized to receive transplant plus maintenance rituximab or maintenance rituximab alone. This trial is something that I talk to every patient about, and I try to get them enrolled.
Individualizing the treatment of MCL has gotten more complicated recently, especially since the presentation of the TRIANGLE trial results. Do we add a BTK inhibitor to chemotherapy at the time of initial diagnosis? Do we still offer patients autologous stem cell transplants at their first remission? The TRIANGLE study results found that the current regimen of intensive chemotherapy is not superior to ibrutinib alone. We have not changed our treatment based on TRIANGLE, however, because the data have not been published yet and because we can no longer get the drug that was actually used in the trial. It is controversial and is causing havoc, so to speak.
When choosing a frontline therapy for a patient with MCL, I consider several things. The first consideration is whether to use aggressive chemotherapy-based treatment. The second is centered around whether the patient has a TP53 mutation. You are not going to be as likely to administer chemotherapy in that scenario given its limited effectiveness. Otherwise, the choice of whether to use intensive chemotherapy in a patient is typically a function of their age and fitness, but some patients prefer to avoid chemotherapy altogether. Some individuals with MCL are older and frail and may not benefit from the high-intensity approaches. Others, even if they are candidates for aggressive treatment, do not want to embark on an intensive chemotherapy-based approach. And then, there are other factors that may be considered in the context of transplant, and the barriers have been well studied, such as a patient’s access to transportation and the availability of a caregiver.
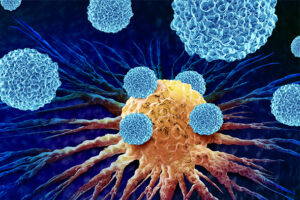
In terms of novel approaches, adding BTK inhibitors and small molecules to the chemotherapy backbone is definitely of interest. It is possible that, with the availability of these agents, chemotherapy may not be needed at all. The early use of CAR T-cell therapy is not standard but is being studied. At present, “cellular therapy” is typically reserved for patients who are receiving autologous stem cell transplantation as first-line therapy, and, typically, CAR T cells are employed as third-line therapy (although earlier use may be considered in certain settings).
ClinicalTrials.gov. ASCT after a rituximab/ibrutinib/Ara-C containing induction in generalized mantle cell lymphoma. Updated December 19, 2017. Accessed November 8, 2023. https://clinicaltrials.gov/study/NCT02858258
ClinicalTrials.gov. Rituximab with or without stem cell transplant in treating patients with minimal residual disease-negative mantle cell lymphoma in first complete remission. Updated June 22, 2023. Accessed November 8, 2023. https://clinicaltrials.gov/study/NCT03267433
Dreyling M, Doorduijn JK, Gine E, et al. Efficacy and safety of ibrutinib combined with standard first-line treatment or as substitute for autologous stem cell transplantation in younger patients with mantle cell lymphoma: results from the randomized TRIANGLE trial by the European MCL Network. Blood. 2022;140(suppl 1):1-3. doi:10.1182/blood-2022-163018
Eskelund CW, Dahl C, Hansen JW, et al. TP53 mutations identify younger mantle cell lymphoma patients who do not benefit from intensive chemoimmunotherapy. Blood. 2017;130(17):1903-1910. doi:10.1182/blood-2017-04-779736
Glimelius I, Smedby KE, Albertsson-Lindblad A, et al. Unmarried or less-educated patients with mantle cell lymphoma are less likely to undergo a transplant, leading to lower survival. Blood Adv. 2021;5(6):1638-1647. doi:10.1182/bloodadvances.2020003645
Kumar A, Eyre TA, Lewis KL, Thompson MC, Cheah CY. New directions for mantle cell lymphoma in 2022. Am Soc Clin Oncol Educ Book. 2022;42:1-15. doi:10.1200/EDBK_349509
Kumar A. What is the role of up-front autologous stem cell transplantation in mantle cell lymphoma? Hematology Am Soc Hematol Educ Program. 2022;2022(1):155-162. doi:10.1182/hematology.2022000333