Oncology
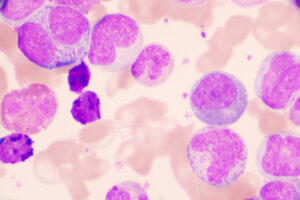
Chronic Lymphocytic Leukemia
Extending Progression-Free and Overall Survival in Chronic Lymphocytic Leukemia
Overview
Long-term data reported at the 63rd ASH Annual Meeting and Exposition reflected advancements in chronic lymphocytic leukemia (CLL), such as improvements in frontline treatment for patients with high-risk disease. Updates on minimal residual disease (MRD)–guided treatment strategies were also among the reports of interest.
Following the conference, featured expert Matthew S. Davids, MD, MMSc, was interviewed by Conference Reporter Editor-in-Chief Tom Iarocci, MD. Dr Davids provides his perspectives on the relevant proceedings here.
Matthew S. Davids, MD, MMSc
|
|
“We have often wondered what we would observe in terms of differences in outcomes in patients who are started on ibrutinib based on del(17p) status. Here, we see that PFS did not differ according to del(17p) status among ibrutinib-treated patients, which is the first time that this has been reported with a BTK inhibitor with long-term follow-up in a prospective trial.”
ASH 2021 was, once again, an important meeting for CLL, and there was some very significant work being presented for the first time. Comparisons of the newer regimens with chemoimmunotherapy (CIT)-based treatment is a good starting point, as we are essentially comparing the old paradigm with the new.
When it was first published in 2018, the practice-changing Alliance A041202 trial found that ibrutinib with or without rituximab was superior to bendamustine plus rituximab (BR) in the first-line setting among older patients with CLL, with regard to progression-free survival (PFS). At ASH 2021, we saw a major update from this trial, with long-term follow-up data (now at 55 months) being reported in abstract 639. It was encouraging and reassuring to see that the ibrutinib arms were still superior to BR with respect to PFS and that the addition of rituximab to ibrutinib did not confer a PFS advantage over ibrutinib alone.
The other very interesting outcome was the PFS in patients with 17p deletion (del[17p]), our highest-risk subset. From past studies we have seen that, in the relapsed/refractory setting, patients with del(17p) respond to ibrutinib but have shorter PFS than those without. We have often wondered what we would observe in terms of differences in outcomes in patients who are started on ibrutinib based on del(17p) status. Here, we see that PFS did not differ according to del(17p) status among ibrutinib-treated patients, which is the first time that this has been reported with a Bruton tyrosine kinase (BTK) inhibitor with long-term follow-up in a prospective trial (abstract 639). Right now, most of us in the field lean toward a continuous BTK inhibitor as initial therapy in the setting of del(17p) and TP53 aberration rather than time-limited therapy with venetoclax plus obinutuzumab.
Results from the phase 3 National Cancer Research Institute FLAIR trial, which compared fludarabine, cyclophosphamide, and rituximab (FCR) with ibrutinib plus rituximab in younger, fit patients, were also presented at ASH 2021 (abstract 642). Researchers reported significant improvements in PFS with ibrutinib plus rituximab, but no overall survival (OS) benefits vs FCR, which I believe supports the idea of continuing to present FCR as a potential option for young, fit patients with mutated IGHV status. At the very least, it brings into question the idea of an OS benefit with ibrutinib plus rituximab over FCR. And the reasons for the discrepant finding as compared with those from the previously published Eastern Cooperative Oncology Group–American College of Radiology Imaging Network (ECOG–ACRIN) Cancer Research Group trial (E1912; NCT02048813), in which an OS benefit with ibrutinib plus rituximab was observed, will be fuel for interesting debate.
Other regimens that are of investigational interest combine novel agents with CIT. For instance, I presented updated data on our ibrutinib-plus-FCR study at ASH 2021 (abstract 640). Now at a median follow-up of approximately 40 months (as compared with the previously published median follow-up data at 16.5 months), we reported a PFS of 97%, and this includes patients with unmutated IGHV who do not typically experience a durable response to FCR alone. So, ibrutinib may be helping in that group in particular. Other studies are showing a similar trend, now with somewhat longer follow-up in young, fit patients (eg, the ICLL07 FILO study from France and the study on ibrutinib, fludarabine, cyclophosphamide, and obinutuzumab from The University of Texas MD Anderson Cancer Center). This suggests that the approach of chemotherapy plus ibrutinib can be highly effective, although we need longer-term follow-up and, ultimately, comparative studies with existing standards of care before this approach can be routinely recommended in practice.
Results with limited-duration venetoclax-based regimens were also of great interest at ASH 2021. The frontline GAIA (CLL13) study is a nearly 1000-patient study that compared 3 different venetoclax-based regimens with CIT, with treatment arms as follows: venetoclax plus rituximab, venetoclax plus obinutuzumab, and venetoclax plus obinutuzumab and ibrutinib (abstract 71). The CIT comparator was either BR or FCR, depending on patient age, whereas prior studies used chlorambucil plus obinutuzumab, a weaker CIT comparator, so these new data were welcomed. We expected the venetoclax regimens to be superior, but the differences were greater than I expected, with high rates of undetectable MRD. The results also confirm that obinutuzumab is a more potent antibody than rituximab and that adding ibrutinib may increase the rate of undetectable MRD, although the difference in rates with or without ibrutinib was not huge (approximately 92% vs approximately 86%). The key with these regimens will be the durability of PFS. We will need longer-term follow-up, given that current results only focus on MRD, but this is an exciting first step.
Two studies evaluating ibrutinib in combination with venetoclax were also updated at the meeting; one in mainly younger, fit patients (CAPTIVATE study; abstract 68) and one in older, less fit patients (GLOW study; abstract 70). Both studies found that the all-oral ibrutinib-plus-venetoclax regimen was highly efficacious, but there was a fair amount of toxicity in the elderly population in GLOW. In contrast, the toxicity profile looked more favorable in the young, fit population in CAPTIVATE.
Trials-in-progress abstracts included the MAJIC study, which is intended to determine the optimal time-limited venetoclax doublet in a broad population of previously untreated patients with CLL (abstract 1553). MAJIC is comparing acalabrutinib plus venetoclax with venetoclax plus obinutuzumab using an MRD-guided strategy. We will evaluate MRD to 10-5 sensitivity by clonoSEQ (Adaptive Biotechnologies) next-generation sequencing, which offers an approximate 10-fold increase in sensitivity over the typical flow-based assays that are used in most trials to date. Patients with detectable MRD after 12 cycles of venetoclax will continue therapy for an additional 12 cycles with either acalabrutinib plus venetoclax or venetoclax monotherapy, for a total of 24 months. The hope is that this approach will allow us to have a greater ability to individualize the duration of therapy. Our study will examine a 2-year duration maximum for the venetoclax-plus-obinutuzumab combination, and understanding the potential benefit of a second year of venetoclax in this setting is currently an important data gap in the field.
Another trial in progress is the ReVenG trial, which is designed to determine the efficacy of a second round of venetoclax plus obinutuzumab in patients who relapsed after first-line venetoclax plus obinutuzumab (abstract 2634). This is a collaboration between our group at the Dana-Farber Cancer Institute and the German CLL Study Group, and we are very interested to know how much clinical benefit there might be from retreatment with this regimen in the setting of progressive disease. So, we expect these trials to help answer many important questions in the coming years.
References
Davids MS, Brander DM, Tyekucheva S, et al. Longer term follow-up of a multicenter, phase 2 study of ibrutinib plus fludarabine, cyclophosphamide, rituximab (iFCR) as initial therapy for younger patients with chronic lymphocytic leukemia [abstract 640]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Davids MS, Fischer K, Robrecht S, et al. ReVenG: a phase 2 study of venetoclax plus obinutuzumab retreatment in patients with relapsed chronic lymphocytic leukemia [abstract 2634]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Davids MS, Mato AR, Hum J, et al. MAJIC: a phase 3 prospective, multicenter, randomized, open-label trial of acalabrutinib plus venetoclax versus venetoclax plus obinutuzumab in previously untreated chronic lymphocytic leukemia or small lymphocytic lymphoma [abstract 1553]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Eichhorst B, Niemann C, Kater AP, et al. A randomized phase III study of venetoclax-based time-limited combination treatments (RVe, GVe, GIVe) vs standard chemoimmunotherapy (CIT: FCR/BR) in frontline chronic lymphocytic leukemia (CLL) of fit patients: first co-primary endpoint analysis of the international intergroup GAIA (CLL13) trial [abstract 71]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Ghia P, Allan JN, Siddiqi T, et al. First-line treatment with ibrutinib (Ibr) plus venetoclax (Ven) for chronic lymphocytic leukemia (CLL): 2-year post-randomization disease-free survival (DFS) results from the minimal residual disease (MRD) cohort of the phase 2 CAPTIVATE study [abstract 68]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Hillmen P, Pitchford A, Bloor A, et al. Ibrutinib plus rituximab is superior to FCR in previously untreated CLL: results of the phase III NCRI FLAIR trial [abstract 642]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Jain N, Thompson P, Burger J, et al. Ibrutinib, fludarabine, cyclophosphamide, and obinutuzumab (iFCG) regimen for chronic lymphocytic leukemia (CLL) with mutated IGHV and without TP53 aberrations. Leukemia. 2021;35(12):3421-3429. doi:10.1038/s41375-021-01280-8
Michallet A-S, Dilhuydy M-S, Subtil F, et al. Obinutuzumab and ibrutinib induction therapy followed by a minimal residual disease–driven strategy in patients with chronic lymphocytic leukaemia (ICLL07 FILO): a single-arm, multicentre, phase 2 trial. Lancet Haematol. 2019;6(9):e470-e479. doi:10.1016/S2352-3026(19)30113-9
Munir T, Moreno C, Owen C, et al. First prospective data on minimal residual disease (MRD) outcomes after fixed-duration ibrutinib plus venetoclax (Ibr+Ven) versus chlorambucil plus obinutuzumab (CLB+O) for first-line treatment of CLL in elderly or unfit patients: the GLOW study [abstract 70]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Shanafelt TD, Wang XV, Kay NE, et al. Ibrutinib-rituximab or chemoimmunotherapy for chronic lymphocytic leukemia. N Engl J Med. 2019;381(5):432-443. doi:10.1056/NEJMoa1817073
Woyach JA, Ruppert AS, Heerema NA, et al. Ibrutinib regimens versus chemoimmunotherapy in older patients with untreated CLL. N Engl J Med. 2018;379(26):2517-2528. doi:10.1056/NEJMoa1812836
Woyach JA, Ruppert AS, Heerema NA, et al. Long-term results of Alliance A041202 show continued advantage of ibrutinib-based regimens compared with bendamustine plus rituximab (BR) chemoimmunotherapy [abstract 639]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American Society of Hematology.