Oncology
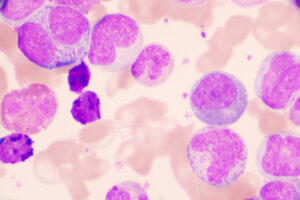
Chronic Lymphocytic Leukemia
Sequencing of Therapies in Chronic Lymphocytic Leukemia
The choice of first-line therapy for chronic lymphocytic leukemia (CLL) may have important implications for subsequent lines of treatment. Initial therapy for CLL in the community is dominated by BTK inhibitor monotherapy, whereas, at large centers, venetoclax plus obinutuzumab is also a commonly used frontline option.
As more data about venetoclax emerge, it is becoming clearer that it can cause clonal hematopoiesis, and it is also associated with significant immune suppression. I consider venetoclax plus obinutuzumab to be like chemoimmunotherapy in that regard.
BTK inhibitors do not cause clonal hematopoiesis, and they cause less immune suppression. Further, progression-free survival benefits extend nicely to patients with high- or low-risk disease with BTK inhibitor therapy. I personally do not recommend venetoclax plus obinutuzumab in the upfront setting unless, for example, a patient has a mechanical heart valve and needs to take warfarin or is very emphatic about receiving time-limited therapy. Many community doctors take this same approach, using upfront covalent BTK inhibitors.
In relapse, I think that venetoclax retreatment is reasonable to consider for patients without Bcl-2 mutations mediating resistance, and it is particularly reasonable for patients who had long remissions with prior venetoclax-based therapy. I would be more likely to re-treat a patient who has been in remission for several years than I would someone who relapsed after less than 1 year off therapy. For patients who relapse between 1 and 2 years after stopping venetoclax-based treatment, my approach depends on the individual patient because data are limited in that setting.
In terms of sequencing, we have much more data ongoing from a BTK inhibitor to venetoclax than the other way around because of the order in which these agents became available, with ibrutinib being introduced long before venetoclax. Some data come from the MURANO trial, which randomized patients with relapsed or refractory CLL to fixed-duration bendamustine and rituximab or venetoclax and rituximab for 2 years. At one point, the trial was amended to allow retreatment with venetoclax, but, by then, many patients had disease progression. As you might expect, almost all of these patients got a BTK inhibitor. But the bottom line is that you can go from venetoclax to a BTK inhibitor or vice versa very effectively.
In the future, if other strategies were to emerge in the front line, this would, of course, impact the conversation on therapeutic sequencing. Today, if we are talking about an antibody, it is obinutuzumab and not rituximab, and we have the newer BTK inhibitors acalabrutinib and zanubrutinib, in addition to ibrutinib. The ongoing, randomized, phase 3 AMPLIFY trial is evaluating the combination of acalabrutinib and venetoclax, with or without obinutuzumab, in patients with previously untreated CLL. If we are going to shift to novel combination therapies up front, the question becomes: Do we really need all 3 agents, or are 2 enough? In other words, if you already have the 2 small molecules on board, is the antibody going to add anything?
We have prospective data with the use of venetoclax-based treatment after BTK inhibition, and not with BTK inhibition after venetoclax-based treatment, but the accumulating experience suggests that there is no problem going from venetoclax to a BTK inhibitor. If you use a BTK inhibitor first and then switch to venetoclax, this is usually in the setting of resistance to the BTK inhibitor, and, in that setting, the benefit from venetoclax lasts for only approximately 2 years. This really worries me in terms of the overall duration of benefit from the therapies. If you use venetoclax first, there is a potential for retreatment, although we have very little data on the success of retreatment. As Dr Byrd alluded to, I think that it is somewhat reasonable to extrapolate from the chemoimmunotherapy era, when patients who had a long remission with their initial chemoimmunotherapy could potentially still benefit from retreatment.
We know from the phase 3 MURANO trial in the relapse setting that some patients with higher-risk CLL can respond to retreatment with venetoclax and rituximab. We do not yet know how long these responses can be, but I suspect that they will be shorter than the first response. Retreatment with time-limited venetoclax regimens may provide additional years of benefit, but we still do not know if this can be done in patients who progress on a BTK inhibitor. I worry that the depth of a second remission will not be the same and that it will be difficult to stop treatment without patients progressing immediately.
I do not recommend using a noncovalent BTK inhibitor in the frontline setting right now, although this is an area of active investigation. Mechanisms of resistance to noncovalent BTK inhibitors involve BTK mutations, and we do not know the full implications of those mutations on subsequent covalent inhibitor use. Since the duration of benefit with covalent BTK inhibitors is long, we would not want to risk losing that benefit based on our limited data with noncovalent BTK inhibitors. And, at the moment, I am fairly neutral about whether noncovalent BTK inhibition should be used before venetoclax or after venetoclax.
Bennett R, Anderson MA, Seymour JF. Unresolved questions in selection of therapies for treatment-naïve chronic lymphocytic leukemia. J Hematol Oncol. 2023;16(1):72. doi:10.1186/s13045-023-01469-7
Blombery P, Lew TE, Dengler MA, et al. Clonal hematopoiesis, myeloid disorders and BAX-mutated myelopoiesis in patients receiving venetoclax for CLL. Blood. 2022;139(8):1198-1207. doi:10.1182/blood.2021012775
ClinicalTrials.gov. Study of acalabrutinib (ACP-196) in combination with venetoclax (ABT-199), with and without obinutuzumab (GA101) versus chemoimmunotherapy for previously untreated CLL. Updated July 20, 2023. Accessed November 9, 2023. https://clinicaltrials.gov/study/NCT03836261
Davids MS, Lampson BL, Tyekucheva S, et al. Acalabrutinib, venetoclax, and obinutuzumab as frontline treatment for chronic lymphocytic leukaemia: a single-arm, open-label, phase 2 study. Lancet Oncol. 2021;22(10):1391-1402. doi:10.1016/S1470-2045(21)00455-1
Hampel PJ, Parikh SA. Chronic lymphocytic leukemia treatment algorithm 2022 [published correction appears in Blood Cancer J. 2022;12(12):172]. Blood Cancer J. 2022;12(11):161. doi:10.1038/s41408-022-00756-9
Kater AP, Harrup R, Kipps TJ, et al. MURANO: final 7 year follow up and retreatment analysis in venetoclax-rituximab (VENR)-treated patients with relapsed/refractory chronic lymphocytic leukemia (R/R CLL) [abstract 156]. Abstract presented at: European Hematology Association Annual Meeting; June 8-11, 2023; Frankfurt, Germany.
Montoya S, Thompson MC. Non-covalent Bruton’s tyrosine kinase inhibitors in the treatment of chronic lymphocytic leukemia. Cancers (Basel). 2023;15(14):3648. doi:10.3390/cancers15143648
Nasnas P, Cerchione C, Musuraca G, et al. How I manage chronic lymphocytic leukemia. Hematol Rep. 2023;15(3):454-464. doi:10.3390/hematolrep15030047
Seymour JF, Kipps TJ, Eichorst B, et al. Venetoclax–rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378(12):1107-1120. doi:10.1056/NEJMoa1713976
Thompson MC, Harrup RA, Coombs CC, et al. Venetoclax retreatment of patients with chronic lymphocytic leukemia after a previous venetoclax-based regimen. Blood Adv. 2022;6(15):4553-4557. doi:10.1182/bloodadvances.2022007812