Oncology
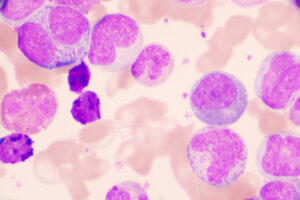
Chronic Lymphocytic Leukemia
Major Unmet Clinical Needs in Chronic Lymphocytic Leukemia
Despite advances in the management of chronic lymphocytic leukemia (CLL), there is still much room for improvement with regard to CLL patient outcomes. Among these unmet needs are improvements in the treatment of Richter’s transformation and treatment strategies for double-refractory patients, younger patients, immunocompromised patients, and patients who develop secondary malignancies.
The treatment of younger patients is an unmet clinical need in CLL. I am reluctant to abandon the fludarabine, cyclophosphamide, and rituximab (FCR) regimen in these patients. I do not think that our other current therapies will allow these younger patients with CLL to achieve their normal life spans. Even those who relapse may potentially get an extra decade of survival with the FCR regimen, although this benefit may be limited to patients receiving frontline FCR treatment. I do not believe that the same benefit can be achieved after patients have progressed on the various targeted therapies, but we do not know that for sure.
In my opinion, the US Food and Drug Administration (FDA) approval rate of newer therapies for CLL will start to slow down, since we do not yet have the evidence that other targets are home runs. Hopefully, we will have some new FDA approvals for the use of the second-generation BTK inhibitors in combination regimens.
Some untreated patients with CLL may never need treatment, but they may require monthly immunoglobulin infusions due to being sufficiently immunocompromised. Treatment for CLL does not usually help restore the immunoglobulin levels in these patients and can sometimes worsen them. There are some patients who, after starting treatment for CLL, require monthly immunoglobulin infusions that were not needed before treatment. I think that the immune restoration component of CLL remains somewhat mysterious and is a major problem.
Patients with CLL are also at an increased risk of secondary malignancies. Secondary malignancies are quite common in the long-term BTK inhibitor clinical trials, and trials are now looking at this problem much more systematically. We do not know the causes of this increased risk. Some people claim that it is related to immune system dysfunction, while others believe that genetic factors could also be involved. I do not think that the problem is therapy related—I think that it is disease related.
A major unmet need in CLL is the treatment of double-refractory patients, meaning patients who are refractory to both BTK inhibitors and venetoclax. These patients progress very quickly and generally do not respond well to conventional therapies. We have learned, however, that some individuals with CLL can be refractory to both BTK inhibitors and venetoclax and then achieve a significant response when both drugs are used in combination. Some patients will achieve a partial or durable remission that can last for several years and then progress and possibly even die 1 or 2 months later. So, we need better treatments for double-refractory patients. Pirtobrutinib received approval from the FDA for patients with mantle cell lymphoma, and we have been able to use it off label in CLL due to the 73.3% overall response rate and 19.6-month median progression-free survival that were seen in the phase 1/2 BRUIN trial. Hopefully, we will have FDA approval for this drug in CLL within the next year.
The treatment of Richter’s transformation is also an unmet need for individuals with CLL. Chimeric antigen receptor T-cell therapy is a promising treatment on the horizon for these patients.
Further, it is clear that COVID-19 has become endemic and is similar to influenza for many of us; however, for patients with CLL, it can be life threatening. Those with CLL generally do not respond well to vaccines, and prophylaxis with tixagevimab plus cilgavimab is no longer effective. So, I think that it is going to be important for these patients that there is continued development of preventive therapies for COVID-19.
Many individuals with CLL who are living longer have received chemotherapy and have issues with therapy-related myeloid neoplasms, including myelodysplastic syndrome and acute myeloid leukemia. We also see an abundance of secondary cancers in these patients that likely come from their immune suppression. Since we are now losing more patients with CLL to secondary cancers, we need to develop more aggressive screening strategies and prevention trials for this population.
Richter’s transformation is the greatest unmet need in terms of the dismal outcomes for these patients, even though they represent only a small fraction of patients with CLL.
Another major unmet need is improved treatments for younger patients with CLL. Remember that the median age of a patient with CLL is approximately 71 years. If I see a 70-year-old patient who is newly diagnosed with CLL, I might start with a watch-and-wait approach. Perhaps the patient will need therapy at age 75 years. I can probably keep this patient with CLL alive long enough for them to die from some other cause. This may be considered a functional cure. But suppose I see a 60-year-old patient with newly diagnosed CLL who is otherwise healthy. Even with all the tools that we have now, can I keep that patient alive long enough to have a normal life span? The answer is no because, eventually, I will run out of treatments.
This situation could change if any of the doublet or triplet regimens, or the VenG combination, which is venetoclax plus obinutuzumab, shows a cure fraction. Remember, the longest follow-up that we have for VenG is 6 years, so, even if there is a cure fraction, it will probably be similar to the cure fraction for FCR. Patients with IGHV mutations are doing very well with VenG, with the CLL14 study reporting a 6-year progression-free survival of approximately 70%. That is great, but it does not tell us if the survival curve will plateau. Patients with CLL are surviving longer, and we need to continually develop newer treatments to allow patients to live normal life spans.
Al-Sawaf O, Robrecht S, Zhang C, et al. Venetoclax-obinutuzumab for previously untreated chronic lymphocytic leukemia: 6-year results of the randomized CLL14 study [abstract S145]. Abstract presented at: European Hematology Association 2023 Congress; June 8-11, 2023; Frankfurt, Germany.
Bond DA, Huang Y, Fisher JL, et al. Second cancer incidence in CLL patients receiving BTK inhibitors. Leukemia. 2020;34(12):3197-3205. doi:10.1038/s41375-020-0987-6
Brown JR, Eichhorst B, Hillmen P, et al. Zanubrutinib or ibrutinib in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2023;388(4):319-332 doi:10.1056/NEJMoa2211582
Byrd JC, Hillmen P, Ghia P, et al. Acalabrutinib versus ibrutinib in previously treated chronic lymphocytic leukemia: results of the first randomized phase III trial. J Clin Oncol. 2021;39(31):3441-3452. doi:10.1200/JCO.21.01210
Fischer K, Al-Sawaf O, Bahlo J, et al. Venetoclax and obinutuzumab in patients with CLL and coexisting conditions. N Engl J Med. 2019;380(23):2225-2236. doi:10.1056/NEJMoa1815281
Fischer K, Bahlo J, Fink AM, et al. Long-term remissions after FCR chemoimmunotherapy in previously untreated patients with CLL: updated results of the CLL8 trial. Blood. 2016;127(2):208-215. doi:10.1182/blood-2015-06-651125
Hyak JM, Huang Y, Rogers KA, et al. Combined BCL2 and BTK inhibition in CLL demonstrates efficacy after monotherapy with both classes. Blood Adv. 2022;6(17):5124-5127. doi:10.1182/bloodadvances.2022007708
Khan S, Allsup D, Molica S. An updated perspective on immunoglobulin replacement in chronic lymphocytic leukaemia in the era of targeted therapies. Front Oncol. 2023;13:1135812. doi:10.3389/fonc.2023.1135812
Mato AR, Davids MS, Sharman J, et al. Recognizing unmet need in the era of targeted therapy for CLL/SLL: “what’s past is prologue” (Shakespeare). Clin Cancer Res. 2022;28:603-608. doi:10.1158/1078-0432.CCR-21-1237
Mato AR, Woyach JA, Brown JR, et al. Pirtobrutinib after a covalent BTK inhibitor in chronic lymphocytic leukemia. N Engl J Med. 2023;389(1):33-44. doi:10.1056/NEJMoa2300696
Parikh SA, Leis JF, Chaffee KG, et al. Hypogammaglobulinemia in newly diagnosed chronic lymphocytic leukemia: natural history, clinical correlates and outcomes. Cancer. 2015;121(17):2883-2891. doi:10.1002/cncr.29438
Smyth E, Eyre TA, Cheah CY. Emerging therapies for the management of Richter transformation. J Clin Oncol. 2023;41(2):395-409. doi:10.1200/JCO.22.01028
Sun C, Wiestner A. Can we restore immunocompetence in CLL? Hematol Oncol Clin North Am. 2021;35(4):827-845. doi:10.1016/j.hoc.2021.03.010