Oncology
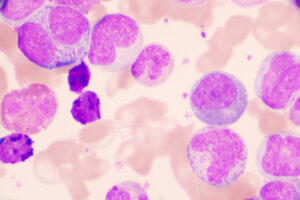
Chronic Lymphocytic Leukemia
Long-term Survival Data With Preferred Frontline Therapies for Chronic Lymphocytic Leukemia
Overview
At the 63rd ASH Annual Meeting and Exposition, updated long-term data were reported from several trials of preferred frontline therapies for chronic lymphocytic leukemia (CLL). Outcomes with the targeted agents are excellent overall compared with chemotherapy-based treatments.
Following these presentations, featured expert Jan A. Burger, MD, PhD, was interviewed by Conference Reporter Editor-in-Chief Tom Iarocci, MD. Dr Burger’s clinical perspectives are presented here.
Jan A. Burger, MD, PhD
|
|
“In summary, with the limited-duration regimen of venetoclax plus obinutuzumab, patients with high-risk CLL have somewhat shorter remissions than with continuous BTK inhibitor therapy; however, outcomes with the targeted agents are excellent overall compared with chemotherapy-based treatments.”
Data on the Bruton tyrosine kinase (BTK) inhibitor ibrutinib go back more than a decade to the phase 1b/2 studies, which included refractory patients and a small cohort of previously untreated patients. The longest follow-up data (ie, up to 8 years) are from a cohort of treatment-naive patients, and they showed that those on ibrutinib monotherapy have extremely good long-term outcomes, with very few progression events. Extended long-term follow-up data are also available from the RESONATE-2 study of first-line ibrutinib vs chlorambucil in older individuals with CLL/small lymphocytic lymphoma. In that study, with up to 7 years of follow-up, ibrutinib continued to perform much better than the chemotherapy-based comparator, and any-grade adverse events leading to discontinuations were observed in 3% of patients from 5 to 6 years and none in 6 to 7 years.
The long-term follow-up data from RESONATE-2 also highlighted that the patients with high-risk CLL derive the same level of benefit from ibrutinib as those with low-risk disease; for example, IGHV-unmutated patients and those with 11q deletion had the same durable remissions as patients with low-risk disease. (Patients with 17p deletion were not included in this study.) An important update from the A041202 trial was presented at ASH 2021 (abstract 639). This phase 3 trial by Woyach et al had previously shown that ibrutinib regimens prolong progression-free survival compared with bendamustine plus rituximab in older patients with treatment-naive CLL. Now with longer follow-up, at a median of 55 months, this group reported in abstract 639 that the benefits of ibrutinib therapy continued to be observed across subgroups, including those linked to higher-risk disease. Further, there did not appear to be inferior progression-free survival for individuals with abnormalities in TP53 who were taking ibrutinib. The authors noted that this finding differentiates ibrutinib, and possibly BTK inhibitors in general, from other targeted therapy paradigms for treatment-naive CLL.
Venetoclax plus obinutuzumab is another very attractive alternative for patients with CLL in the frontline setting. Most data on the frontline use of venetoclax come from the CLL14 trial from the German CLL Study Group. Updated data from CLL14 were reported earlier this year by Al-Sawaf et al. Venetoclax plus obinutuzumab differs from BTK inhibitor therapy in that it is a limited-duration treatment, whereby patients receive venetoclax orally for 1 year and are given intravenous obinutuzumab for the first 6 months. Then, at the end of the year, they stop treatment entirely and are monitored. With longer follow-up, after 3 to 4 years, we see that patients are starting to relapse. Relapses after venetoclax plus obinutuzumab are occurring particularly in those with 17p deletion, but also in patients who are IGHV unmutated. Thus, if we treat high-risk patients with this limited-duration treatment, we must watch them closely after a few years for any sign of relapse.
In the research setting, novel combinations for CLL are now being evaluated, and these newer combinations are being compared with single-agent BTK inhibitors or with venetoclax, which traditionally has always been given with CD20 antibodies. We are just starting to hear about some of these combinations at ASH 2021 (eg, abstracts 68 and 71), and the rationale behind this work is to induce deeper remissions.
In summary, with the limited-duration regimen of venetoclax plus obinutuzumab, patients with high-risk CLL have somewhat shorter remissions than with continuous BTK inhibitor therapy; however, outcomes with the targeted agents are excellent overall compared with chemotherapy-based treatments. Novel combinations (eg, a BTK inhibitor plus venetoclax) are likely to further improve on these outcomes and may open the door for more use of limited-duration treatment.
References
Al-Sawaf O, Zhang C, Robrecht S, et al. Venetoclax-obinutuzumab for previously untreated chronic lymphocytic leukemia: 4-year follow-up analysis of the randomized CLL14 study [abstract S146]. Abstract presented at: European Hematology Association 2021 Virtual Congress; June 9-17, 2021.
Barr PM, Owen C, Robak T, et al. Up to seven years of follow-up in the RESONATE-2 study of first-line ibrutinib treatment for patients with chronic lymphocytic leukemia. J Clin Oncol. 2021;39(suppl 15):7523. doi:10.1200/JCO.2021.39.15_suppl.7523
Byrd JC, Furman RR, Coutre SE, et al. Ibrutinib treatment for first-line and relapsed/refractory chronic lymphocytic leukemia: final analysis of the pivotal phase Ib/II PCYC-1102 study. Clin Cancer Res. 2020;26(15):3918-3927. doi:10.1158/1078-0432.CCR-19-2856
Eichhorst B, Niemann C, Kater AP, et al. A randomized phase III study of venetoclax-based time-limited combination treatments (RVe, GVe, GIVe) vs standard chemoimmunotherapy (CIT: FCR/BR) in frontline chronic lymphocytic leukemia (CLL) of fit patients: first co-primary endpoint analysis of the international intergroup GAIA (CLL13) trial [abstract 71]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Ghia P, Allan JN, Siddiqi T, et al. First-line treatment with ibrutinib (Ibr) plus venetoclax (Ven) for chronic lymphocytic leukemia (CLL): 2-year post-randomization disease-free survival (DFS) results from the minimal residual disease (MRD) cohort of the phase 2 CAPTIVATE study [abstract 68]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Woyach JA, Ruppert AS, Heerema NA, et al. Ibrutinib regimens versus chemoimmunotherapy in older patients with untreated CLL. N Engl J Med. 2018;379(26):2517-2528. doi:10.1056/NEJMoa1812836
Woyach JA, Ruppert AS, Heerema NA, et al. Long-term results of Alliance A041202 show continued advantage of ibrutinib-based regimens compared with bendamustine plus rituximab (BR) chemoimmunotherapy [abstract 639]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the American Society of Hematology.