Rheumatology
Systemic Lupus Erythematosus
Systemic Lupus Erythematosus Roundup at Eastern Rheumatology Congress
Overview
The introduction of novel therapies has provided new treatment options for patients with systemic lupus erythematosus (SLE) and lupus nephritis. Researchers at the 2023 Congress of Clinical Rheumatology (CCR) East presented data on the effectiveness and safety of these agents from several studies aiming to address the unmet needs of patients with SLE.
Following these presentations, featured expert Maureen A. McMahon, MD, was interviewed by Christopher Ontiveros, PhD. Dr McMahon’s clinical perspectives are presented here.
Maureen A. McMahon, MD
|
|
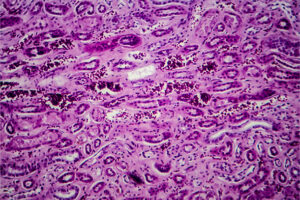
There were a number of presentations and posters at this year's CCR East that were relevant to the treatment of patients with SLE. In particular, the talk by Michelle Petri, MD, MPH, on newer therapies for SLE was a highlight. She reiterated the importance of using hydroxychloroquine as background therapy in all patients with SLE, as it has been shown to improve survival. In those with lupus nephritis, Dr Petri emphasized the importance of treating earlier and more aggressively, pointing out that the percentage of nephrons that are lost even in the first episode of lupus nephritis can be substantial. Thus, I appreciated the algorithm that she outlined for high-risk patients. This approach included the consideration of dual therapy right from the start. And then, for those who do not achieve at least a 25% improvement by 12 weeks, the consideration of therapeutic escalation; for those who do not achieve a 50% improvement by 6 months, once again, the consideration of escalation.
In the last few years, the newer therapies belimumab and voclosporin have been approved by the US Food and Drug Administration (FDA) for add-on therapy in lupus nephritis, and we are trying to determine the best time to add these treatments to the current induction regimens of mycophenolate or cyclophosphamide plus corticosteroids, or whether we should start triple therapy at the beginning. Dr Petri also reviewed data from the phase 3 AURORA trials, which found that the addition of voclosporin to mycophenolate and corticosteroids was associated with significantly greater improvements in renal outcomes compared with mycophenolate and steroids alone.
Regarding posters that were presented at CCR East, a post hoc analysis by Caster et al of voclosporin in class V lupus nephritis using 3 years of data from the AURORA 1 and the AURORA 2 studies demonstrated that the addition of voclosporin was associated with a substantial and faster reduction in urine protein to creatinine ratios vs mycophenolate and low-dose steroids alone. In addition, in their 2-year safety follow-up of patients from the original AURORA 2 study, Saxena and colleagues found no unexpected safety signals with the addition of voclosporin over 3 years of treatment when compared with patients who were continued on mycophenolate and low-dose steroids. While these were not prospective studies, the results provide additional reassurance that we can safely use voclosporin over extended periods.
There were also several posters at CCR East that addressed the use of belimumab. For example, a real-world study of claims data by Bell et al found that adherence to belimumab was linked to a significantly lower rate of SLE flares relative to standard therapy. Additionally, a post hoc analysis of 5 phase 3 trials by Manzi et al suggested that the addition of belimumab produced improvements in mucocutaneous manifestations of SLE compared with standard therapy, with a particularly strong signal for patients with vasculitis.
Regarding SLE-associated cardiovascular disease, first, I would note that there are plenty of data that suggest that lupus nephritis may have an adverse impact on cardiovascular disease; therefore, by treating lupus nephritis more effectively, I think that our patients will ultimately gain in both arenas. But there was a really interesting case presentation by Vadlamudi and colleagues at CCR East about atherosclerosis in SLE involving a 34-year-old patient who had had lupus since the age of 13. This patient presented with myocardial infarction and was found to have a lesion in her right coronary artery. The case really reminds us that our patients with SLE are at higher cardiovascular risk, including our younger patients with SLE. Right now, I think that our best strategies to mitigate cardiovascular risk include trying to target any modifiable cardiac risk factors that we can (eg, cholesterol, tobacco use, and hypertension, among other factors). Prednisone can increase some of those modifiable risk factors, so steroids are definitely one of the medications that we should be aggressively trying to minimize.
Some data suggest that some of the same mechanisms that are responsible for lupus disease activity, including B cells and the interferon pathway, might also be involved in driving cardiovascular risk in lupus, so, as we collect more data over time, it will be interesting to see whether newly FDA-approved therapies for lupus, such as anifrolumab or belimumab, may have beneficial effects in preventing cardiovascular disease—above and beyond just the steroid-sparing effects.
Overall, the availability of these effective new options is resulting in a paradigm shift for how aggressively we are approaching the management of lupus and lupus nephritis. In my practice, I am certainly more aggressive at treating nephritis than I used to be. For instance, for high-risk patients, I will introduce the idea of dual therapy at the onset, and I am more aggressive about changing or adding on therapies when the treatment has not been effective.
References
Bell CF, Rubin B, Worley K, et al. Real-world effectiveness of belimumab in patients with systemic lupus erythematosus in the United States. Poster presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Caster DJ, Saxena A, Almaani S, Rosales A, Leher H. Long-term use of voclosporin in patients with class V lupus nephritis: results from the AURORA 2 continuation study. Poster presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Dall'Era M, Cisternas MG, Smilek DE, et al. Predictors of long-term renal outcome in lupus nephritis trials: lessons learned from the Euro-Lupus Nephritis cohort. Arthritis Rheumatol. 2015;67(5):1305-1313. doi:10.1002/art.39026
Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78(6):736-745. doi:10.1136/annrheumdis-2019-215089
Manzi S, Sanchez-Guerrero J, Yokogawa N, et al. Belimumab effects on skin in patients with systemic lupus erythematosus, a pooled post hoc analysis of five phase 3, randomized, placebo-controlled clinical trials. Poster presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Morand EF, Furie R, Tanaka Y, et al; TULIP-2 Trial Investigators. Trial of anifrolumab in active systemic lupus erythematosus. N Engl J Med. 2020;382(3):211-221. doi:10.1056/NEJMoa1912196
Petri M. Comparison of new therapies for SLE. Presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Saxena A, Teng O, Collins C, England N, Leher H. Voclosporin for lupus nephritis: results of the two-year AURORA 2 continuation study. Poster presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
Tumurkhuu G, Montano E, Jefferies C. Innate immune dysregulation in the development of cardiovascular disease in lupus. Curr Rheumatol Rep. 2019;21(9):46. doi:10.1007/s11926-019-0842-9
Vadlamudi K, Hasan S, Hayat S. An intersection between lupus and myocardial infarction. Poster presented at: 2023 Congress of Clinical Rheumatology East; May 4-7, 2023; Destin, FL.
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the Congress of Clinical Rheumatology.