Oncology
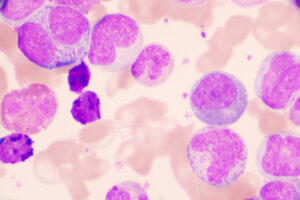
Chronic Lymphocytic Leukemia
Current Treatment Options for Older Patients With Relapsed/Refractory Chronic Lymphocytic Leukemia
Overview
The treatment approach in older patients with relapsed/refractory chronic lymphocytic leukemia (CLL) is evolving due to the emergence of novel agents and new regimens—and, particularly, their incorporation into frontline regimens.
Q: How do you treat the older patient with relapsed/refractory CLL in the current treatment era?
Jennifer R. Brown, MD, PhD
|
|
“For older patients who are relapsing after some form of CIT, the primary options would be either ibrutinib therapy, for which we have the most data, or venetoclax-rituximab as a 2-year, limited-duration regimen.”
The approach to treatment of older patients with relapsed/refractory CLL is primarily guided by prior therapies, the durability of remissions, and the presence of comorbidities. For older patients who are relapsing after some form of chemoimmunotherapy (CIT), the primary options would be either ibrutinib therapy, for which we have the most data, or venetoclax-rituximab as a 2-year, limited-duration regimen. Follow-up is not quite as long for venetoclax-rituximab, but Seymour et al reported that, at 3 years, most patients who had discontinued treatment as planned at 2 years were able to remain in remission over the following year, with only approximately 13% of patients progressing. Of these, most had 17p deletion/TP53 mutation at baseline or detectable minimal residual disease (MRD) at the end of the 2 years. Deciding between ibrutinib and venetoclax-rituximab in older patients is based, in part, on the presence of comorbidities and on tolerability. I have spoken with community oncologists who found that ibrutinib was more difficult to give than they had expected based on the findings of published trials, but I think that practitioners are becoming more familiar with it now, and that is helpful. With ibrutinib, I worry about cardiac toxicity, particularly among patients who have congestive heart failure or low ejection fraction. Venetoclax is usually very well tolerated after the initial ramp-up, but there is a risk of tumor lysis syndrome, especially among those with reduced renal function and high white blood cell counts or high tumor burden. If a patient has severe cardiac and renal comorbidity, phosphoinositide 3 (PI3) kinase inhibitors can be well tolerated despite those comorbidities. For the increasing proportion of patients who have received ibrutinib as first-line therapy, venetoclax is the clear choice for those who progress. We can still get a high response rate and some durability in these individuals. For those patients who stopped ibrutinib because of adverse events, one might consider using PI3 kinase inhibitors, and antibodies could be used for those with a low disease burden or an autoimmune complication.
Bruce D. Cheson, MD, FACP, FAAAS, FASCO
|
|
“There have been enormous shifts in treatment over the last few years, with fewer older patients with CLL receiving CIT. Most patients now receive ibrutinib-based therapy up front.”
There have been enormous shifts in treatment over the last few years, with fewer older patients with CLL receiving CIT. Most patients now receive ibrutinib-based therapy up front. Older individuals are certainly not getting fludarabine-cyclophosphamide-rituximab, fewer and fewer are getting bendamustine-rituximab (BR) up front, and they are only rarely getting chlorambucil. We have had data on ibrutinib for 7 to 8 years now. The use of upfront ibrutinib in the older patient has been studied in the Alliance North American Intergroup Study A041202, which found that ibrutinib alone is superior to BR in terms of progression-free survival, although overall survival was not significantly different. The safety profile of the ibrutinib-based arms was superior to BR in terms of hematologic toxicities; however, the grade 3 and above nonhematologic adverse events were more prevalent in the ibrutinib-containing arms, including unwitnessed grade 5 adverse events, so close monitoring is important and toxicity might limit the use of Bruton’s tyrosine kinase inhibition in the entire population of older patients. In addition to the increased risk of atrial fibrillation in patients with ibrutinib, there is also an increased risk of hypertension, which is not an infrequent complication. Ibrutinib-induced hypertension can present as either new onset or worsening of existing hypertension. For patients who have relapsed following ibrutinib, the preferred treatment is venetoclax or venetoclax-rituximab. It is important to emphasize that ibrutinib should not be stopped abruptly; it should be continued in those who are progressing until you have transitioned them to a second-line therapy. PI3 kinase inhibitors are not often used. Idelalisib-rituximab was approved by the US Food and Drug Administration for relapsed CLL and is used for both older patients and for those who are unlikely to tolerate CIT well because of compromised bone marrow, renal failure, and poor performance status. With respect to the sequencing of agents, we do have data showing that venetoclax is extremely effective in patients who have progressed on ibrutinib, but we have very limited data on the converse. CIT is of limited benefit in the relapse setting.
Susan O’Brien, MD
|
|
“When I use venetoclax for relapsed/refractory CLL, I use it in combination with rituximab. The combination of venetoclax with ibrutinib is associated with significantly better outcomes vs single-agent venetoclax, and rituximab is easy to administer and is generally well tolerated, even in older patients.”
I agree that the approach to treatment is influenced by the first-line treatment and that the primary options for those who relapse following a CIT regimen are ibrutinib or venetoclax with or without rituximab. A PI3 kinase inhibitor (eg, duvelisib, idelalisib) may also be considered. I would be hesitant to use ibrutinib in a patient who is receiving anticoagulation. A recent study looking at the aggregated risk of major bleeding in patients on ibrutinib found that there was no increased risk of major hemorrhage vs control after adjustments for time on drug. Nevertheless, although the risk appears to be low and the use of anticoagulation is not an absolute contraindication, there would be a hesitation to use ibrutinib in these patients. If ibrutinib was still considered the best choice for a patient requiring anticoagulation, an option would be to use a non–vitamin K novel oral anticoagulant that has less of a risk of bleeding compared with warfarin. Although there is an increased use of ibrutinib over CIT regimens such as BR, some community oncologists are still inclined to use BR as frontline therapy. Although this is not my approach, the mindset that you often see in the community is that, since you are not likely to cure the disease, you can buy approximately 4 years before you have to go to another agent. When I use venetoclax for relapsed/refractory CLL, I use it in combination with rituximab. The combination of venetoclax with ibrutinib is associated with significantly better outcomes (particularly with respect to MRD negativity) vs single-agent venetoclax, and rituximab is easy to administer and is generally well tolerated, even in older patients.
References
Brown JR, Moslehi J, Ewer MS, et al. Incidence of and risk factors for major haemorrhage in patients treated with ibrutinib: an integrated analysis. Br J Haematol. 2019;184(4):558-569.
Cuneo A, Foà R. Management of CLL in the elderly. Ann Oncol. 2017;28(2):200-204.
Ordovás Baines JP, Climent Grana E, Jover Botella A, Valero García I. Pharmacokinetics and pharmacodynamics of the new oral anticoagulants dabigatran and rivaroxaban [in Spanish]. Farm Hosp. 2009;33(3):125-133.
Seymour JF, Kipps TJ, Eichhorst B, et al. MURANO trial establishes feasibility of time-limited venetoclax-rituximab (VenR) combination therapy in relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL). Presented at: 60th American Society of Hematology Annual Meeting & Exposition; December 1-4, 2018; San Diego, CA. Abstract 184.
Seymour JF, Kipps TJ, Eichhorst B, et al. Venetoclax-rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378(12):1107-1120.
Shustik C, Bence-Bruckler I, Delage R, Owen CJ, Toze CL, Coutre S. Advances in the treatment of relapsed/refractory chronic lymphocytic leukemia. Ann Hematol. 2017;96(7):1185-1196.
Thompson PA, O'Brien SM, Wierda WG, et al. Complex karyotype is a stronger predictor than del(17p) for an inferior outcome in relapsed or refractory chronic lymphocytic leukemia patients treated with ibrutinib-based regimens. Cancer. 2015;121(20):3612-3621.
Woyach JA, Ruppert AS, Heerema NA, et al. Ibrutinib regimens versus chemoimmunotherapy in older patients with untreated CLL. N Engl J Med. 2018;379(26):2517-2528.