Oncology
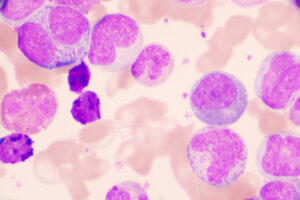
Chronic Lymphocytic Leukemia
Exploring the Next-Generation Small-Molecule Inhibitors for Chronic Lymphocytic Leukemia
Overview
Small-molecule inhibitors have transformed the treatment of chronic lymphocytic leukemia (CLL). The rationale for new drug development is to build on the successes of agents such as ibrutinib and venetoclax while reducing toxicities.
Expert Commentary
William G. Wierda, MD, PhD
|
|
“While venetoclax is very effective, it can be associated with tumor lysis syndrome, and mitigation strategies make initiation and escalation to the target dose cumbersome. So, an agent with the efficacy of venetoclax but with less risk for tumor lysis syndrome could have an advantage.”
The next generation of small-molecule inhibitors for CLL has already begun to emerge, with second-generation Bruton tyrosine kinase (BTK) inhibitors such as acalabrutinib receiving approval from the US Food and Drug Administration (FDA). The rationale for new drug development is to build on the successes of agents such as ibrutinib and venetoclax while reducing toxicities.
Ibrutinib has transformed the CLL treatment landscape, but some of its side effects, even when they are not grade 3 or higher, can become significant issues for patients on continuous and indefinite therapy. These include diarrhea, arthralgia, and myalgia, and they seem to be less of an issue with acalabrutinib than with ibrutinib. Many of us who use these drugs regularly do prefer acalabrutinib over ibrutinib because of the reduction in these lower-grade toxicities, as well as the lower incidence of atrial fibrillation. However, it is important to keep in mind that there is still some risk of cardiac issues and toxicities with all of the currently available irreversible BTK inhibitors. That is, reduced toxicity is not zero toxicity.
Thus far, the BTK inhibitors that are available have been irreversible inhibitors. On the horizon, we have pirtobrutinib (LOXO-305), a reversible BTK inhibitor that has shown very promising activity in heavily pretreated patients, including those who were refractory to irreversible inhibitors and those who have the mutation that is associated with irreversible BTK inhibitor resistance (ie, cysteine 481). Pirtobrutinib is well tolerated, with no dose-limiting toxicities identified in the phase 1 study. I am very optimistic about pirtobrutinib for patients with CLL who are developing refractory disease, although we still need longer-term follow-up to demonstrate the durability of these responses.
The development of novel BCL-2 inhibitors has been a bit more complex. There are compounds that are under investigation, but I have not yet seen evidence to suggest any mechanistic advantages over venetoclax in terms of efficacy, although some molecules that are under study may have a more favorable toxicity profile. There is no single pervasive mutation linked to venetoclax resistance, and other mechanisms of resistance are likely relevant, such as increased expression of MCL-1 or BCL-xL. While venetoclax is very effective, it can be associated with tumor lysis syndrome, and mitigation strategies make initiation and escalation to the target dose cumbersome. So, an agent with the efficacy of venetoclax but with less risk for tumor lysis syndrome could have an advantage.
Regarding the phosphoinositide 3-kinase (PI3K) inhibitors, idelalisib has demonstrated activity in treating relapsed/refractory CLL, but its use has been limited by toxicities. Duvelisib is FDA approved for relapsed/refractory CLL, and it may be better tolerated than idelalisib. Phase 3 data for another novel agent in this class, umbralisib, combined with the novel CD20 antibody ublituximab in first-line and relapsed CLL is currently under review by the FDA. Umbralisib seems to be well tolerated, but the progression-free survival in the first-line setting appears to be shorter than one would expect to see with irreversible BTK inhibitors. So, the use of PI3Kδ inhibitors may still be relegated to later lines.
References
Ailawadhi S, Chanan-Khan AAA, Chen Z, et al. First-in-human study of lisaftoclax (APG-2575), a novel BCL-2 inhibitor (BCL-2i), in patients (pts) with relapsed/refractory (R/R) CLL and other hematologic malignancies (HMs) [abstract 7502]. Abstract presented at: 2021 American Society of Clinical Oncology Annual Meeting; June 4-8, 2021.
Gribben JG, Jurczak W, Jacobs R, et al. Umbralisib plus ublituximab (U2) is superior to obinutuzumab plus chlorambucil (O+Chl) in patients with treatment naïve (TN) and relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL): results from the phase 3 Unity-CLL study [abstract 543]. Abstract presented at: 62nd American Society of Hematology Annual Meeting and Exposition; December 5-8, 2020.
Lunning M, Vose J, Nastoupil L, et al. Ublituximab and umbralisib in relapsed/refractory B-cell non-Hodgkin lymphoma and chronic lymphocytic leukemia. Blood. 2019;134(21):1811-1820. doi:10.1182/blood.2019002118
Maharaj K, Powers JJ, Achille A, et al. The dual PI3Kδ/CK1ε inhibitor umbralisib exhibits unique immunomodulatory effects on CLL T cells. Blood Adv. 2020;4(13):3072-3084. doi:10.1182/bloodadvances.2020001800
Mato AR, Ghosh N, Schuster SJ, et al. Phase 2 study of the safety and efficacy of umbralisib in patients with CLL who are intolerant to BTK or PI3Kδ inhibitor therapy. Blood. 2021;137(20):2817-2826. doi:10.1182/blood.2020007376
Mato AR, Shah NN, Jurczak W, et al. Pirtobrutinib in relapsed or refractory B-cell malignancies (BRUIN): a phase 1/2 study. Lancet. 2021;397(10277):892-901. doi:10.1016/S0140-6736(21)00224-5
Patel K, Pagel JM. Exploring a future for PI3K inhibitors in chronic lymphocytic leukemia. Curr Hematol Malig Rep. 2019;14(4):292-301. doi:10.1007/s11899-019-00525-9
Woyach JA, Rogers KA, Bhat SA, et al. Acalabrutinib with obinutuzumab (Ob) in treatment-naive (TN) and relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL): three-year follow-up. J Clin Oncol. 2019;37(suppl 15):7500. doi:10.1200/JCO.2019.37.15_suppl.750