Oncology
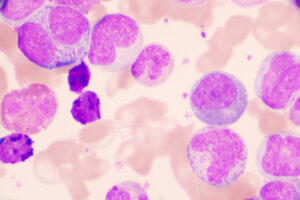
Chronic Lymphocytic Leukemia
High-Risk Chronic Lymphocytic Leukemia: TP53 Aberrancy in Focus
Overview
Chronic lymphocytic leukemia (CLL) with TP53 aberrancy represents a high-risk subset for which optimal therapy has yet to be defined. Combination treatments incorporating second-generation Bruton tyrosine kinase (BTK) inhibitor therapies are being explored in clinical trials.
What are your thoughts on the treatment of TP53-aberrant CLL?
John C. Byrd, MD
|
|
“In thinking about high-risk CLL as an investigator, I would be more excited about adding TP53-independent agents to a BTK inhibitor with or without a CD20 antibody, as opposed to adding venetoclax.”
Venetoclax as a monotherapy, or even when administered with obinutuzumab, does not look very good in the high-risk CLL subset. With the addition of a BTK inhibitor, results are certainly better, but I think that this is an important investigational area. The combination of a BTK inhibitor plus venetoclax, if approved by the US Food and Drug Administration, may be of interest; however, we do not know which, if any, of the combinations that are under consideration will have durable remissions in patients with high-risk CLL.
Aberrant p53 functioning is often associated with genomic instability. It makes sense that the more of an unstable clone that remains after treatment, the greater the chances of resistance, so I think that the eradication of disease will be important. Drawing on data from other B-cell malignancies, we have learned about a variety of mutations that are relatively rare in CLL but may still be informative. Some mutations seem to signal the ability to partially bypass a BTK inhibitor; there is a rare translocation that causes the overexpression of BCL3 and activates the NF-κB pathway. Other mutations, such as CARD11, are observed more in patients with diffuse large B-cell lymphoma, and BTK inhibitors appear to be effective.
This situation provides an opportunity to consider other targeted drugs, drug combinations, and enrollment in a clinical trial. In thinking about high-risk CLL as an investigator, I would be more excited about adding TP53-independent agents to a BTK inhibitor with or without a CD20 antibody, as opposed to adding venetoclax. Such agents might be something broader than venetoclax, to hit not only BCL2 but also bcl-xL or several of the BCL2 family members.
Ian W. Flinn, MD, PhD
|
|
“The current data appear to be better with continuous BTK inhibitor therapy than with the time-limited approach of venetoclax.”
For most patients with either a TP53 mutation or 17p deletion (del[17p]), I recommend a BTK inhibitor and not venetoclax plus obinutuzumab as frontline treatment. The current data appear to be better with continuous BTK inhibitor therapy than with the time-limited approach of venetoclax. One confounding issue is the duration of therapy. It is possible that you might have better outcomes in high-risk populations if you give venetoclax for a longer period of time. In the phase 3 MURANO trial, venetoclax was given for a longer period. In this relapsed or refractory CLL population, venetoclax plus rituximab resulted in significantly higher rates of progression-free survival than bendamustine plus rituximab. Further, the 2-year progression-free survival rate among those with del(17p) was 81.5% in the venetoclax-plus-rituximab group vs 27.8% in the bendamustine-plus-rituximab group. These results appear better to me than what you might expect with a shorter duration of treatment.
Additionally, I agree with Dr Byrd that we simply do not know which combinations will produce the best outcomes in our high-risk populations. I would go even further to say that we do not yet know which 2- or 3-drug combinations will be best in any of the treatment settings that are being considered, but I am fairly confident that a BTK inhibitor should be incorporated in the first-line treatment of patients with del(17p).
Jeff Sharman, MD
|
|
“There is still reasonable uncertainty in the field regarding the optimal treatment strategy for patients with these genetic mutations.”
There is still reasonable uncertainty in the field regarding the optimal treatment strategy for patients with these genetic mutations. I also tend to favor a BTK inhibitor–based approach in patients with del(17p), and, for the time being, that would be primarily BTK inhibitor monotherapy.
We are currently exploring acalabrutinib with either venetoclax or obinutuzumab in the phase 3 MAJIC trial. Additionally, interim data from the phase 3 ALPINE trial comparing the second-generation BTK inhibitor zanubrutinib with ibrutinib in adults with relapsed or refractory CLL look very promising. Of those on zanubrutinib, 11.6% had del(17p) and 8.2% had TP53 mutations; of those on ibrutinib, 12.5% had del(17p) and 5.8% had TP53 mutations. Researchers reported that zanubrutinib significantly improved response rates and delayed disease progression compared with ibrutinib. For the poor prognosis subset of patients with del(17p), the overall response rate was significantly higher with zanubrutinib compared with ibrutinib (83.3% vs 53.8%). Encouragingly, substantially lower rates of atrial fibrillation/flutter and cardiac disorders of any grade were reported with zanubrutinib than with ibrutinib. Finally, in general, when I look at the data from the phase 3 CLL14 trial of venetoclax plus obinutuzumab, I see that patients with del(17p) tended to have earlier relapses.
References
Al-Sawaf O, Zhang C, Tandon M, et al. Venetoclax plus obinutuzumab versus chlorambucil plus obinutuzumab for previously untreated chronic lymphocytic leukaemia (CLL14): follow-up results from a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2020;21(9):1188-1200. doi:10.1016/S1470-2045(20)30443-5
ClinicalTrials.gov. A study of acalabrutinib plus venetoclax versus venetoclax plus obinutuzumab in previously untreated chronic lymphocytic leukemia or small lymphocytic lymphoma (MAJIC). Updated January 19, 2022. Accessed March 9, 2022. https://www.clinicaltrials.gov/ct2/show/NCT05057494
Davids MS, Mato AR, Hum J, et al. MAJIC: a phase 3 prospective, multicenter, randomized, open-label trial of acalabrutinib plus venetoclax versus venetoclax plus obinutuzumab in previously untreated chronic lymphocytic leukemia or small lymphocytic lymphoma [abstract 1553]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Davids MS, Waweru C, Le Nouveau P, et al. Comparative efficacy of acalabrutinib in frontline treatment of chronic lymphocytic leukemia: a systematic review and network meta-analysis. Clin Ther. 2020;42(10):1955-1974.e15. doi:10.1016/j.clinthera.2020.08.017
Hallek M. Chronic lymphocytic leukemia: 2017 update on diagnosis, risk stratification, and treatment. Am J Hematol. 2017;92(9):946-965. doi:10.1002/ajh.24826
Hillmen P, Eichhorst BF, Brown JR, et al. First interim analysis of ALPINE study: results of a phase 3 randomized study of zanubrutinib vs ibrutinib in patients with relapsed/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma [abstract LB1900]. Abstract presented at: European Hematology Association 2021 Virtual Congress; June 9-17, 2021.
O'Brien S, Furman RR, Coutre S, et al. Single-agent ibrutinib in treatment-naïve and relapsed/refractory chronic lymphocytic leukemia: a 5-year experience. Blood. 2018;131(17):1910-1919. doi:10.1182/blood-2017-10-810044
Seymour JF, Kipps TJ, Eichhorst B, et al. Venetoclax–rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378(12):1107-1120. doi:10.1056/NEJMoa1713976
Sharman JP, Egyed M, Jurczak W, et al. Acalabrutinib with or without obinutuzumab versus chlorambucil and obinutuzmab for treatment-naive chronic lymphocytic leukaemia (ELEVATE-TN): a randomised, controlled, phase 3 trial [published correction appears in Lancet. 2020;395(10238):1694]. Lancet. 2020;395(10232):1278-1291. doi:10.1016/S0140-6736(20)30262-2
Smith CIE, Burger JA. Resistance mutations to BTK inhibitors originate from the NF-κB but not from the PI3K-RAS-MAPK arm of the B cell receptor signaling pathway. Front Immunol. 2021;12:689472. doi:10.3389/fimmu.2021.689472
Stefaniuk P, Onyszczuk J, Szymczyk A, Podhorecka M. Therapeutic options for patients with TP53 deficient chronic lymphocytic leukemia: narrative review. Cancer Manag Res. 2021;13:1459-1476. doi:10.2147/CMAR.S283903
Tam CS, Trotman J, Opat S, et al. Phase 1 study of the selective BTK inhibitor zanubrutinib in B-cell malignancies and safety and efficacy evaluation in CLL. Blood. 2019;134(11):851-859. doi:10.1182/blood.2019001160