Oncology
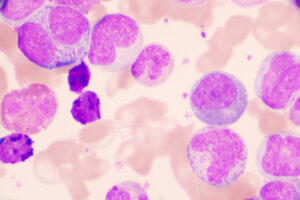
Chronic Lymphocytic Leukemia
Minimal Residual Disease Negativity in Chronic Lymphocytic Leukemia
Overview
Minimal residual disease (MRD) negativity after chemoimmunotherapy is associated with improved progression-free and overall survival in patients with chronic lymphocytic leukemia (CLL). However, the significance of MRD negativity is not yet clear with respect to novel therapies that act through differing mechanisms. Indeed, ibrutinib has demonstrated conclusive overall survival benefit in randomized trials without achieving MRD negativity. Our featured experts, Jennifer R. Brown, MD, PhD, Jan A. Burger, MD, PhD, and Anthony Mato, MD, MSCE, consider MRD negativity in CLL from different perspectives.
Q: What is the significance of MRD negativity in CLL? Please discuss its use as an end point in clinical trials.
Anthony R. Mato, MD, MSCE
|
|
“It is also important to note that the risk-benefit ratio of various treatment regimens can differ greatly, and, for individual patients, maintaining a good quality of life with excellent control of CLL may be of greater importance than achieving MRD negativity.”
In chemoimmunotherapy trials, complete response (by International Workshop on Chronic Lymphocytic Leukemia criteria) and achievement of MRD status is correlated with prolonged progression-free and overall survival. So, while MRD negativity may be a clinically important end point in potentially curative strategies, MRD analysis is not a part of routine practice in the current standard of care. It is also important to note that the risk-benefit ratio of various treatment regimens can differ greatly, and, for individual patients, maintaining a good quality of life with excellent control of CLL may be of greater importance than achieving MRD negativity.
Jennifer R. Brown, MD, PhD
|
|
“MRD negativity also depends on the type of therapy because it is a post-therapy measure rather than something that we assess prior to starting treatment.”
MRD negativity also depends on the type of therapy because it is a post-therapy measure rather than something that we assess prior to starting treatment. As Dr Mato noted, with chemoimmunotherapy, MRD negativity as measured by 4-color flow cytometry is quite predictive of better progression-free and overall survival. It seems likely that MRD negativity is also important in the setting of venetoclax therapy, although the extent of the data is not as great. It is really with the B-cell receptor pathway inhibitors, including ibrutinib and idelalisib, where the role of MRD negativity has not been established, and it is rare when patients have been treated with single agents or even with single agents plus antibody.
Jan A. Burger, MD, PhD
|
|
“MRD negativity is also used as an end point in clinical trials investigating combination therapy. For example, at the last American Society of Hematology Annual Meeting and Exposition, there was discussion of early data from a trial investigating the combination of ibrutinib and venetoclax for high-risk patients, and there the goal is to achieve MRD negativity in a high fraction of patients.”
MRD negativity is also used as an end point in clinical trials investigating combination therapy. For example, at the last American Society of Hematology Annual Meeting and Exposition, there was discussion of early data from a trial investigating the combination of ibrutinib and venetoclax for high-risk patients, and there the goal is to achieve MRD negativity in a high fraction of patients. The data are premature at this point, so all that we can say is that, based on high response rates and MRD negativity, it looks like a promising strategy, but we do not have progression-free survival data at this point for combinations of a Bruton’s tyrosine kinase inhibitor with a B-cell lymphoma-2 antagonist that show superiority to sequential therapy.
References
Böttcher S, Hallek M, Ritgen M, Kneba M. The role of minimal residual disease measurements in the therapy for CLL: is it ready for prime time? Hematol Oncol Clin North Am. 2013;27(2):267-288.
Cheson BD, Byrd JC, Rai KR, et al. Novel targeted agents and the need to refine clinical end points in chronic lymphocytic leukemia. J Clin Oncol. 2012;30(23):2820-2822.
Hallek M, Cheson BD, Catovsky D, et al. Guidelines for diagnosis, indications for treatment, response assessment and supportive management of chronic lymphocytic leukemia. Blood. 2018 Mar 14. pii: blood-2017-09-806398. doi: 10.1182/blood-2017-09-806398. [Epub ahead of print]
Hallek M, Shanafelt TD, Eichhorst B. Chronic lymphocytic leukaemia. Lancet. 2018;391(10129):1524-1537.
Hillmen P, Munir T, Rawstron A, et al. Initial results of ibrutinib plus venetoclax in relapsed, refractory CLL (Bloodwise TAP CLARITY study): high rates of overall response, complete remission and MRD eradication after 6 months of combination therapy. Abstract 428. Presented at: 59th ASH Annual Meeting and Exposition; December 9-12, 2017; Atlanta, GA.
Shustik C, Bence-Bruckler I, Delage R, Owen CJ, Toze CL, Coutre S. Advances in the treatment of relapsed/refractory chronic lymphocytic leukemia. Ann Hematol. 2017;96(7):1185-1196.