Oncology
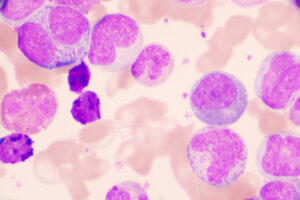
Chronic Lymphocytic Leukemia
Most Effective Outcome Measures for Assessing Treatment Response in Relapsed/Refractory Chronic Lymphocytic Leukemia
Overview
The most useful outcome measures in chronic lymphocytic leukemia (CLL) are dependent on the treatment regimen. In general, progression-free survival (PFS) is the gold standard for assessing response in patients with CLL.
Q: What are the most effective outcome measures for assessing treatment response in relapsed/refractory CLL?
Susan O’Brien, MD
|
|
“Novel therapies such as ibrutinib have changed the way we think about response.”
Historically, with chemoimmunotherapy (CIT), we looked at PFS, which is important. We also looked at response, particularly complete response (CR), because we know that CR correlates with longer PFS when you are using CIT. With ibrutinib, you rarely get a CR and you are certainly not talking about minimal residual disease (MRD). And yet, despite this, you have these very durable remissions. So, novel therapies such as ibrutinib have changed the way we think about response. With CIT, we saw that patients with CRs were generally going to have a longer remission than those who only achieved partial responses—but this is not the case with ibrutinib. It is also true that when you see an early response to ibrutinib, that does not necessarily give you an early indication of how well the patient is going to respond over the long-term. With venetoclax, it is slightly different if you are aiming for MRD in that the advantage of MRD negativity is that it can allow you to consider treatment discontinuation. However, in older patients with CLL, you are likely not as concerned with achieving MRD negativity because they have a significantly shorter lifespan. The improvement of symptoms is also an important consideration with small molecules. In general, most patients with CLL respond fairly quickly (within the first few months of therapy), although there are some individuals who do not respond until after several months of therapy or who respond slowly over the course of 1 year or even longer.
Jennifer R. Brown, MD, PhD
|
|
“The most appropriate outcome measurement depends on the type of therapy. For BTK inhibitors such as ibrutinib, PFS is what we need to be looking at.”
PFS is likely our main gold standard at this point, since our trials are resulting in a prolonged PFS. Overall survival (OS) is a long time frame in CLL, and there are effective salvage regimens in most cases, which makes it difficult to evaluate that end point. But the most appropriate outcome measurement depends on the type of therapy. For Bruton tyrosine kinase (BTK) inhibitors such as ibrutinib, PFS is what we need to be looking at. Overall response rates with these agents are extremely high, but CR rates are generally low and undetectable MRD is unlikely, although PFS is quite long. It would be useful to obtain more data on how CR impacts PFS; the only data that we currently have in this setting are in the 17p deletion group, based on very few patients. In contrast to BTK inhibition, undetectable MRD and CR are strongly correlated with PFS with CIT and with venetoclax. With ibrutinib-venetoclax regimens, quite a few patients are achieving CR and undetectable MRD, but we do not know anything about PFS yet. This is an area that needs proper assessment. The only way to compare time-limited regimens with something that is continuous (eg, single-agent ibrutinib) is through the assessment of PFS or OS. Since the regimens have differential effects on CR and undetectable MRD that may be correlated with PFS for one drug but not the other, you cannot make that comparison based on CR or undetectable MRD.
Bruce D. Cheson, MD, FACP, FAAAS, FASCO
|
|
“If clinicians start using MRD negativity as a threshold for stopping treatment, they must be cautious about what assay they are actually using and what the sensitivity is, otherwise there will be unsuspected and unpredicted recurrences.”
I agree that the ideal outcome measures are context dependent. CLL is different from other hematologic malignancies in which OS may be more useful. PFS is quite useful in CLL, but there are also important caveats. If you are going to use PFS to compare regimens, you want a therapy that improves PFS but is relatively nontoxic and inexpensive. If you are calling a therapy “superior” based on improved PFS, this generally assumes that you also have at least comparable—or preferably improved—quality of life. So, in varying circumstances, other end points may be preferable. If feasible, shorter durations of therapy are preferable from a cost and cumulative toxicity standpoint.
With respect to MRD negativity as an end point, one has to be careful about its measurement. Numerous assays with differing sensitivities are available, and there is a significant difference between MRD negativity in blood vs bone marrow. If you have MRD negativity with a blood assay that has a sensitivity of 10-4 and then you use a bone marrow assay in the same patient that has a 10-6 sensitivity, there is a good chance that your patient who was MRD negative by blood assay will become MRD positive by bone marrow. Thus, if clinicians start using MRD negativity as a threshold for stopping treatment, they must be cautious about what assay they are actually using and what the sensitivity is, otherwise there will be unsuspected and unpredicted recurrences. In short, there is a lack of standardization in this area, although we are getting closer with currently available assays such as the clonotypic assays. If the goal is cure, we should be using the most sensitive assay in clinical trials. The one scenario in which using a blood assay is appropriate is when your patient’s blood is positive; in this case, you do not need to do anything further. If the patient’s blood becomes negative, however, you must look at the bone marrow, the more sensitive assay.
References
Byrd JC, Hillmen P, O’Brien S, et al. Long-term follow-up of the RESONATE™ phase 3 trial of ibrutinib versus ofatumumab. Blood. 2019 Mar 6. pii: blood-2018-08-870238. doi: 10.1182/blood-2018-08-870238. [Epub ahead of print]
Cheson BD, Byrd JC, Rai KR, et al. Novel targeted agents and the need to refine clinical end points in chronic lymphocytic leukemia. J Clin Oncol. 2012;30(23):2820-2822.
Hallek M, Cheson BD, Catovsky D, et al. iwwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131(25):2745-2760.
Moreno C, Greil R, Demirkan F, et al. Ibrutinib plus obinutuzumab versus chlorambucil plus obinutuzumab in first-line treatment of chronic lymphocytic leukaemia (iLLUMINATE): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(1):43-56.
Owen C, Christofides A, Johnson N, Lawrence T, MacDonald D, Ward C. Use of minimal residual disease assessment in the treatment of chronic lymphocytic leukemia. Leuk Lymphoma. 2017;58(12):2777-2785.
Pal Singh S, Dammeijer F, Hendriks RW. Role of Bruton's tyrosine kinase in B cells and malignancies [published correction appears in Mol Cancer. 2019;18(1):79]. Mol Cancer. 2018;17(1):57.
Thompson M, Brander D, Nabhan C, Mato A. Minimal residual disease in chronic lymphocytic leukemia in the era of novel agents: a review. JAMA Oncol. 2018;4(3):394-400.
Warren CFA, Wong-Brown MW, Bowden NA. BCL-2 family isoforms in apoptosis and cancer. Cell Death Dis. 2019;10(3):177.