Oncology
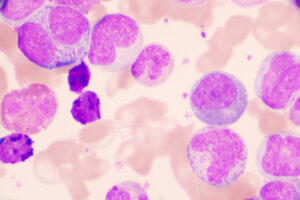
Chronic Lymphocytic Leukemia
Novel Agents and Combinations for Treatment-Naive Chronic Lymphocytic Leukemia
Overview
Several novel agent–based combinations are being evaluated in the frontline setting for chronic lymphocytic leukemia (CLL). Regimens that include time-limited therapy and/or the inclusion of second-generation agents with improved toxicity profiles hold great promise.
What are some of the considerations with investigational regimens that are of interest in the frontline setting for CLL?
Matthew S. Davids, MD, MMSc
|
|
“ . . . acalabrutinib is a better-tolerated BTK inhibitor than ibrutinib, and that may be particularly important when combining with other agents.”
There are 3 main ways in which novel agent combinations could be used going forward in treatment-naive CLL. The first is to combine a novel agent with chemoimmunotherapy. For example, the addition of ibrutinib to fludarabine, cyclophosphamide, and rituximab (iFCR regimen) or to fludarabine, cyclophosphamide, and obinutuzumab (iFCG regimen) has produced promising results. The second category is a novel agent plus an antibody. We now have 4-year data from the CLL14 study in which venetoclax plus obinutuzumab was associated with a progression-free survival rate of 74%. The third and, in my opinion, most interesting category is the use of novel/novel combinations. The US cancer cooperative groups are comparing the ibrutinib, venetoclax, and obinutuzumab (IVO) regimen to ibrutinib plus obinutuzumab. An Eastern Cooperative Oncology Group study is comparing these combinations in younger, fit patients, while an Alliance for Clinical Trials in Oncology trial is evaluating these combinations in an older cohort with comorbidities.
Based on data that were recently presented on the ibrutinib-plus-venetoclax combination in older patients in the GLOW study, it may be challenging for older patients to tolerate the IVO regimen. I am more optimistic about acalabrutinib paired with venetoclax either with or without obinutuzumab. Based on data from ELEVATE-RR, we recently saw that acalabrutinib is a better-tolerated Bruton tyrosine kinase (BTK) inhibitor than ibrutinib, and that may be particularly important when combining with other agents. To that end, we recently published our data from a phase 2 study of the combination of acalabrutinib plus venetoclax and obinutuzumab, which was found to be well tolerated with a high rate of undetectable minimal residual disease (MRD). This regimen is now being compared to acalabrutinib plus venetoclax and to chemoimmunotherapy in a phase 3 trial. We are also about to open the MAJIC trial (NCT05057494) in which we will compare what we consider the current standard of care for time-limited therapy (venetoclax plus obinutuzumab) with acalabrutinib plus venetoclax, which is an all-oral regimen and what we think could be a great option for patients in the future. A novel aspect of our study is that the duration of therapy in both arms will be guided by next-generation sequencing-based MRD testing.
Susan O’Brien, MD
|
|
“All combinations that are under evaluation include venetoclax combined with either a BTK inhibitor or a PI3K inhibitor. Most trials are using a BTK inhibitor because of the known toxicities with extended therapy with PI3K inhibitors.”
All combinations that are under evaluation include venetoclax combined with either a BTK inhibitor or a phosphoinositide 3-kinase (PI3K) inhibitor. Most trials are using a BTK inhibitor because of the known toxicities with extended therapy with PI3K inhibitors. For example, the CAPTIVATE trial is examining the use of a time-limited regimen that involves 3 months of lead-in with ibrutinib and then 12 months of ibrutinib plus venetoclax. Data from the 2021 American Society of Clinical Oncology Annual Meeting showed that this regimen was associated with undetectable MRD in 77% of patients in peripheral blood and 60% in bone marrow with a 24-month progression-free survival of 95%. We are very excited about these high rates of MRD undetectability. Whether the addition of an antibody to this regimen will improve outcomes is an open question.
I think that novel agents plus chemotherapy are also potentially relevant. For example, The University of Texas MD Anderson Cancer Center has evaluated the use of chemoimmunotherapy substituting obinutuzumab for rituximab in previously untreated patients with mutated IGHV and no 17p deletion or TP53 mutation. The regimen lowered the number of cycles to 3 and added ibrutinib. The rationale was that perhaps we could preserve some of the outcomes associated with FCR (ie, the plateau lasting >16 years in the mutated group that indicates cure) while decreasing toxicity.
William G. Wierda, MD, PhD
|
|
“My preference is moving away from chemotherapy, particularly alkylating agent–based treatment, because, even with a reduced number of cycles of chemotherapy, we are still seeing cases of secondary MDS and AML in patients on our clinical trials.”
My preference is moving away from chemotherapy, particularly alkylating agent–based treatment, because, even with a reduced number of cycles of chemotherapy, we are still seeing cases of secondary myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) in patients on our clinical trials. We have a trial that we refer to as iFCG that enrolled patients who have a mutated immunoglobulin gene with a goal of giving less chemotherapy while achieving a higher rate of undetectable MRD and, perhaps, a higher cure rate than what we saw with FCR in this subgroup. With iFCG, patients received 3 cycles of fludarabine and cyclophosphamide with 12 cycles of ibrutinib and 6 to 12 cycles of obinutuzumab.
We have observed a higher rate of undetectable MRD with iFCG than we saw with FCR, but, in the cohort of 45 patients treated with iFCG, we have seen 1 or 2 cases of MDS, and that is with the 3 cycles of FC, rather than 6 cycles that we use with standard FCR. So, we are still seeing some MDS, even with reduced chemotherapy exposure. And I think that, given that we have such effective targeted therapies with very high undetectable MRD rates and clinical remissions with what seems to be less risk for secondary MDS and AML, I am favoring moving away from chemoimmunotherapy. Even though it is a low percentage of patients who are getting MDS or AML, I am still uncomfortable with that risk, particularly in young individuals, and therefore I am moving away from recommending chemotherapy-based treatment in favor of targeted therapy.
References
Al-Sawaf O, Zhang C, Robrecht S, et al. Venetoclax-obinutuzumab for previously untreated chronic lymphocytic leukemia: 4-year follow-up analysis of the randomized CLL14 study [abstract S146]. Abstract presented at: European Hematology Association 2021 Virtual Congress; June 9-17, 2021.
Byrd JC, Hillmen P, Ghia P, et al. Acalabrutinib versus ibrutinib in previously treated chronic lymphocytic leukemia: results of the first randomized phase III trial. J Clin Oncol. 2021 Jul 25:JCO2101210. doi:10.1200/JCO.21.01210
ClinicalTrials.gov. A study of acalabrutinib plus venetoclax versus venetoclax plus obinutuzumab in previously untreated chronic lymphocytic leukemia or small lymphocytic lymphoma (MAJIC). Accessed October 7, 2021. https://clinicaltrials.gov/ct2/show/NCT05057494
ClinicalTrials.gov. Ibrutinib and obinutuzumab with or without venetoclax in treating patients with chronic lymphocytic leukemia. Accessed October 7, 2021. https://clinicaltrials.gov/ct2/show/NCT03701282
ClinicalTrials.gov. Testing the addition of a new anti-cancer drug, venetoclax, to the usual treatment (ibrutinib and obinutuzumab) in untreated, older patients with chronic lymphocytic leukemia. Accessed October 7, 2021. https://clinicaltrials.gov/ct2/show/NCT03737981?term=NCT03737981&draw=2&rank=1
Davids MS, Brander DM, Kim HT, et al; Blood Cancer Research Partnership of the Leukemia & Lymphoma Society. Ibrutinib plus fludarabine, cyclophosphamide, and rituximab as initial treatment for younger patients with chronic lymphocytic leukaemia: a single-arm, multicentre, phase 2 trial. Lancet Haematol. 2019;6(8):e419-e428. doi:10.1016/S2352-3026(19)30104-8
Davids MS, Lampson BL, Tyekucheva S, et al. Acalabrutinib, venetoclax, and obinutuzumab as frontline treatment for chronic lymphocytic leukaemia: a single-arm, open-label, phase 2 study. Lancet Oncol. 2021;22(10):1391-1402. doi:10.1016/S1470-2045(21)00455-1
Ghia P, Allan JN, Siddiqi T, et al. Fixed-duration (FD) first-line treatment (tx) with ibrutinib (I) plus venetoclax (V) for chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL): primary analysis of the FD cohort of the phase 2 captivate study. J Clin Oncol. 2021;39(suppl 15):7501. doi:10.1200/JCO.2021.39.15_suppl.7501
Jain N, Thompson P, Burger J, et al. Ibrutinib, fludarabine, cyclophosphamide, and obinutuzumab (iFCG) regimen for chronic lymphocytic leukemia (CLL) with mutated IGHV and without TP53 aberrations. Leukemia. 2021 May 18. doi:10.1038/s41375-021-01280-8
Kater A, Owen C, Moreno C, et al. Fixed-duration ibrutinib and venetoclax (I+V) versus chlorambucil plus obinutuzumab (CLB+O) for first-line (1L) chronic lymphocytic leukemia (CLL): primary analysis of the phase 3 GLOW study [abstract LB1902]. Abstract presented at: European Hematology Association 2021 Virtual Congress; June 9-17, 2021.
Michallet A-S, Letestu R, Le Garff-Tavernier M, et al. A fixed-duration, measurable residual disease-guided approach in CLL: follow-up data from the phase 2 ICLL-07 FILO trial. Blood. 2021;137(8):1019-1023. doi:10.1182/blood.2020008164
Sharman JP, Egyed M, Jurczak W, et al. Acalabrutinib with or without obinutuzumab versus chlorambucil and obinutuzmab for treatment-naive chronic lymphocytic leukaemia (ELEVATE TN): a randomised, controlled, phase 3 trial [published correction appears in Lancet. 2020;395(10238):1694]. Lancet. 2020;395(10232):1278-1291. doi:10.1016/S0140-6736(20)30262-2
Woyach JA, Blachly JS, Rogers KA, et al. Acalabrutinib in combination with venetoclax and obinutuzumab or rituximab in patients with treatment-naïve or relapsed/refractory chronic lymphocytic leukemia [abstract 1312]. Abstract presented at: 62nd American Society of Hematology Annual Meeting and Exposition; December 5-8, 2020.
Woyach J, Ruppert AS, Perez G, et al. Alliance A041702: a randomized phase III study of ibrutinib plus obinutuzumab versus ibrutinib plus venetoclax and obinutuzumab in untreated older patients (≥70 years of age) with chronic lymphocytic leukemia (CLL). Blood. 2019;134(suppl 1):1751. doi:https://doi.org/10.1182/blood-2019-127102