Oncology
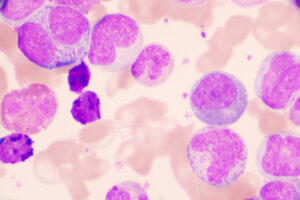
Chronic Lymphocytic Leukemia
Overcoming Immunodeficiency in Chronic Lymphocytic Leukemia
Overview
Patients with chronic lymphocytic leukemia (CLL) are complicated in their humoral and cellular immunodeficiency. While no CLL therapy is viewed as “infection neutral,” important differences exist between regimens that are more myelosuppressive and those that are not.
Q: With respect to overcoming immunodeficiency, how should CLL and its treatments be viewed?
Bruce D. Cheson, MD, FACP, FAAAS, FASCO
|
|
“I am not sure that there is a single statement that fits all patients because patients with CLL are complicated in their humoral and cellular immunodeficiency.”
CLL is a disorder of dysfunctional lymphocytes such that patients are at an increased risk of developing all sorts of infections owing to various immune deficits, marrow infiltration, hypogammaglobulinemia, and complement defects. In patients with CLL, particularly those with advanced-stage disease, there is increased bone marrow involvement in addition to other defects in humoral and cellular immunity. When you add immunosuppressive drugs such as fludarabine (and, to a lesser extent, bendamustine), which can decrease T cells for a prolonged period of time, you are further increasing the risk of infections; we have seen that in clinical trials when fludarabine-cyclophosphamide-rituximab is compared with bendamustine-rituximab or with ibrutinib. We frequently administer intravenous immunoglobulin (Ig) to patients who have recurrent bacterial infections. There are some data demonstrating that the kinase inhibitors may improve certain aspects of a patient’s immune function, but there are also data showing that they increase the risk of opportunistic infections, perhaps because of an impact on the macrophages. I am not sure that there is a single statement that fits all patients because patients with CLL are complicated in their humoral and cellular immunodeficiency. The close monitoring of patients and swift reactions if infection is suspected are required because of the risk of serious or life-threatening opportunistic infections, particularly with the use of ibrutinib. I think an important point to make is that things are changing extremely fast in CLL, so one has to draw the treatment algorithms in pencil because it seems as if a new regimen is approved or a new study comes out every couple of months that shifts things.
Susan O’Brien, MD
|
|
“Several studies suggest that ibrutinib enhances chimeric antigen receptor T-cell function and that improved T-cell function may also contribute to the efficacy of ibrutinib in CLL.”
Whether there are any CLL therapies that are neutral with respect to infection risk is an interesting question, and the data are not easy to analyze. Before the start of any treatment for CLL, the rate of serious infections is elevated compared with the general population. There were 2 cohorts in the original phase 2 trial for ibrutinib: the heavily pretreated patients and the older frontline patients. The cumulative incidence of infection in relapsed/refractory patients was upwards of 40%, which is significant. However, I would argue that much of that risk was related to heavy pretreatment for CLL and not to ibrutinib. The fact that the pretreatment produced some of the infection risk is supported by the much lower rate of infection in the older patients receiving frontline ibrutinib (ie, at 5 years, most of the infection cases were observed in relapsed/refractory patients). So, the presence of disease and/or prior therapy can predispose people to infection, irrespective of the therapy that they are receiving. With any small molecule, there is certainly less immunosuppression and less myelosuppression than chemotherapy. Whether these agents are immune restorative is an open question. Several studies suggest that ibrutinib enhances chimeric antigen receptor T-cell function and that improved T-cell function may also contribute to the efficacy of ibrutinib in CLL. There are really no data for venetoclax in this regard. Another difference between chemotherapy and small molecules is that many clinicians will use prophylactic antibiotics when using chemotherapy, but usually not when using small molecules, with the possible exception of prophylaxis for varicella zoster. There is no specific surveillance pattern for infection in patients with CLL. Primarily, we inform these individuals that they do not have a completely normal immune system, and we ask them to contact us if they become ill.
Jennifer R. Brown, MD, PhD
|
|
“I generally do not view any therapy as being truly infection neutral or as having the capacity to improve the risk of infection.”
I have started to notice more patients becoming hypogammaglobulinemic as their disease progresses, so this is something that we need to be cognizant of as we observe cases. In the study by Mauro et al, 899 patients with stage A CLL were retrospectively analyzed. Low levels of IgG were recorded in approximately 20% of patients at presentation, low levels of IgM and/or IgA were recorded in 10.4% of patients at presentation, and an additional 20% of patients developed hypogammaglobulinemia during the course of the disease. Before the start of any treatment, approximately 13% of patients experienced at least one infection that was grade 3 or above that required a systemic anti-infective treatment and/or hospitalization. They also found that stage A patients with clinical and biologic characteristics of a more aggressive disease more frequently develop late-onset hypogammaglobulinemia and infections that are grade 3 and above and require closer clinical monitoring. I generally do not view any therapy as being truly infection neutral or as having the capacity to improve the risk of infection, so I am always particularly careful to monitor for infection when initiating any new therapy and I frequently use Pneumocystis jiroveci pneumonia and varicella zoster virus prophylaxis in patients with CLL receiving any therapy. I would parallel Dr O’Brien’s comment about infection rates in clinical trials being most related to the disease setting, noting that venetoclax data generally suggest lower infection rates than ibrutinib or idelalisib, but the rates are still significant as they are from relapsed/refractory patients. In considering whether therapy actually improves immune function, one aspect to look at that has not, to my knowledge, been done is to investigate whether patients are able to successfully come off of intravenous Ig. I have not yet seen any data reporting on this.
References
Byrd JC, Furman RR, Coutre SE, et al. Three-year follow-up of treatment-naïve and previously treated patients with CLL and SLL receiving single-agent ibrutinib. Blood. 2015;125(16):2497-2506.
Davids MS, Hallek M, Wierda W, et al. Comprehensive safety analysis of venetoclax monotherapy for patients with relapsed/refractory chronic lymphocytic leukemia. Clin Cancer Res. 2018;24(18):4371-4379.
Fraietta JA, Beckwith KA, Patel PR, et al. Ibrutinib enhances chimeric antigen receptor T-cell engraftment and efficacy in leukemia. Blood. 2016;127(9):1117-1127.
Long M, Beckwith K, Do P, et al. Ibrutinib treatment improves T cell number and function in CLL patients. J Clin Invest. 2017;127(8):3052-3064.
Mauro FR, Morabito F, Vincelli ID, et al. Clinical relevance of hypogammaglobulinemia, clinical and biologic variables on the infection risk and outcome of patients with stage A chronic lymphocytic leukemia. Leuk Res. 2017;57:65-71.
O’Brien S, Furman RR, Coutre S, et al. Single-agent ibrutinib in treatment-naïve and relapsed/refractory chronic lymphocytic leukemia: a 5-year experience. Blood. 2018;131(17):1910-1919.
Schliffke S, Sivina M, Kim E, et al. Dynamic changes of the normal B lymphocyte repertoire in CLL in response to ibrutinib or FCR chemo-immunotherapy. Oncoimmunology. 2018;7(4):e1417720.