Oncology
Endometrial Cancer
Quality of Life in Patients With Endometrial Cancer
Overview
Minimally invasive surgical approaches and adjuvant brachytherapy for patients with high-intermediate-risk endometrioid cancer are among the advances that may have a positive impact on quality of life (QOL).
Expert Commentary
Alexander B. Olawaiye, MD, FRCOG, FACOG, FACS
|
|
“Most patients with endometrioid tumors have negative lymph nodes, and the cancer is usually stage IA or IB. Women in this group generally have an excellent survival rate and do not require adjuvant therapy. Once they recover from surgery, they are able to move on with their lives and have an excellent QOL.”
Of course, receiving a diagnosis of cancer can impact one's QOL. But, beyond that, the type of endometrial cancer, its stage, and its treatment, along with the associated side effects of treatment, are all factors that can influence health-related QOL. Health-related QOL has been studied in the 12 months after initial treatment, and it is clear, for instance, that having multiple comorbidities and having advanced tumor stage can be important factors that may result in a patient requiring more support.
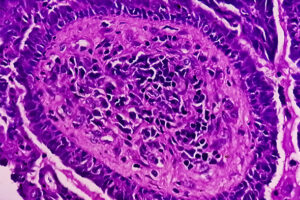
In general, endometrial cancers are divided into 2 broad groups: endometrioid and nonendometrioid tumors. Endometrioid tumors account for approximately 70% to 80% of cases and are graded using the International Federation of Gynecology and Obstetrics (FIGO) grading system. In contrast, nonendometrioid tumors affect approximately 20% of patients. Nonendometrioid tumor types include endometrial serous carcinoma, clear cell carcinoma, and carcinosarcoma. Endometrial serous carcinoma is the most common of the nonendometrioid tumors and is often associated with extrauterine disease.
For a patient with endometrioid histology, surgery alone is usually sufficient and, in most cases, may cure the patient without additional therapy. For most women with endometrial cancer, surgical approaches today include the laparoscopic or robotic removal of the uterus, cervix, fallopian tubes, and ovaries, as well as sentinel lymph node evaluation. These minimally invasive surgeries are associated with advantages over the traditional open abdominal approach, such as lower rates of postoperative complications.
Most patients with endometrioid tumors have negative lymph nodes, and the cancer is usually stage IA or IB. Women in this group generally have an excellent survival rate and do not require adjuvant therapy. Once they recover from surgery, they are able to move on with their lives and have an excellent QOL. The rest of those with stage I disease can be categorized into low-intermediate-risk, high-intermediate-risk, and high-risk subgroups on the basis of age, tumor grade, histologic features, extent of myometrial invasion, and presence or absence of lymphovascular space invasion. Those in the high-intermediate-risk category are now generally offered adjuvant brachytherapy. Patients who receive adjuvant brachytherapy tend to have a good QOL because it is typically given in 3 to 5 treatments and is performed by vaginal cylinder insertion, and morbidity is really minimal.
If a patient has stage IV disease, we generally avoid radiation therapy and just give chemotherapy. Six cycles of chemotherapy or full pelvic radiation can significantly impact QOL. On the chemotherapy side, a very common and important side effect is peripheral neuropathy, which can be quite challenging and debilitating for women who experience it. On the radiation side, patients can experience side effects that include vaginal narrowing, which affects their sexual lives, and problems with bowels (eg, radiation-induced bowel obstruction). Secondary malignancies can also develop as a result of radiation therapy. Any of these events can significantly impact a woman’s QOL.
References
Ferguson SE, Panzarella T, Lau S, et al. Prospective cohort study comparing quality of life and sexual health outcomes between women undergoing robotic, laparoscopic and open surgery for endometrial cancer. Gynecol Oncol. 2018;149(3):476-483. doi:10.1016/j.ygyno.2018.04.558
Forsse D, Barbero ML, Werner HMJ, et al. Longitudinal effects of adjuvant chemotherapy and lymph node staging on patient-reported outcomes in endometrial cancer survivors: a prospective cohort study. Am J Obstet Gynecol. 2022;226(1):90.e1-90.e20. doi:10.1016/j.ajog.2021.08.011
Glasspool R, Wheelwright S, Bolton V, et al. Modifiable pre-treatment factors are associated with quality of life in women with gynaecological cancers at diagnosis and one year later: results from the HORIZONS UK national cohort study. Gynecol Oncol. 2022;165(3):610-618. doi:10.1016/j.ygyno.2022.03.012
Karabuga H, Gultekin M, Tulunay G, et al. Assessing the quality of life in patients with endometrial cancer treated with adjuvant radiotherapy. Int J Gynecol Cancer. 2015;25(8):1526-1533. doi:10.1097/IGC.0000000000000509
Lu KH, Broaddus RR. Endometrial cancer. N Engl J Med. 2020;383(21):2053-2064. doi:10.1056/NEJMra1514010
Tung H-J, Huang H-J, Lai C-H. Adjuvant and post-surgical treatment in endometrial cancer. Best Pract Res Clin Obstet Gynaecol. 2022;78:52-63. doi:10.1016/j.bpobgyn.2021.06.002
Walker JL, Piedmonte MR, Spirtos NM, et al. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27(32):5331-5336. doi:10.1200/JCO.2009.22.3248
Zandbergen N, de Rooij BH, Vos MC, et al. Changes in health-related quality of life among gynecologic cancer survivors during the two years after initial treatment: a longitudinal analysis. Acta Oncol. 2019;58(5):790-800. doi:10.1080/0284186X.2018.1560498