Oncology
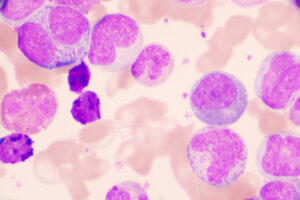
Chronic Lymphocytic Leukemia
Recommendations for the Use of Maintenance and Consolidation Therapy in Chronic Lymphocytic Leukemia
Overview
With the emergence of novel agents for the treatment of chronic lymphocytic leukemia (CLL), the focus has shifted away from the concept of post-chemoimmunotherapy (post-CIT) consolidation and maintenance (eg, lenalidomide-antibody). Moreover, a number of limited-duration, novel-agent combinations are currently being explored in clinical trials.
Q: What roles do consolidation/maintenance therapies have in CLL?
Jennifer R. Brown, MD, PhD
|
|
“Despite some data, there has not been much traction for these maintenance or consolidation strategies.”
In terms of post-CIT and lenalidomide-antibody maintenance, I think that an advantage of CIT is its time-limited nature. With maintenance, you are giving that away and getting cumulative toxicity without survival benefit. That is why, despite some data, there has not been much traction for these maintenance or consolidation strategies. Some of the interest in this topic may stem from clinicians who want to administer ibrutinib for 6 to 12 months and then stop. Discontinuing ibrutinib after 6 to 12 months is not supported by the data as a planned strategy. Ibrutinib must be continued for as long as possible per patient tolerability.
Data for a number of time-limited therapies are emerging. The venetoclax-rituximab regimen from the phase 3 MURANO trial, which is now a registered regimen, was a 2-year, time-limited therapy plan in which venetoclax was continued for 2 years unless disease progression or unacceptable toxic effects occurred sooner. The early relapses appear to be enriched for those with 17p deletion or high levels of detectable minimal residual disease. These data are preliminary, but, if confirmed, the findings could inform some of the decisions about how long to continue treatment vs when to stop treatment. Venetoclax-obinutuzumab is another upfront 1-year, time-limited therapy that appears to have promise; however, only preliminary data have been published. There was also a study by a group in the United Kingdom that found that the addition of obinutuzumab in a delayed fashion in patients who had already achieved significant cytoreduction from ibrutinib was associated with a greater increase in complete response rates and undetectable minimal residual disease. This result was likely related to the pharmacokinetics of antibodies. Since antibodies are cleared by the disease burden, waiting to introduce the drug until the disease burden is reduced may result in a better response and may allow you to consider discontinuation. With respect to ibrutinib combinations, the ongoing, randomized UK FLAIR trial, which is comparing fludarabine-cyclophosphamide-rituximab, ibrutinib-rituximab, ibrutinib-venetoclax, and ibrutinib monotherapy in previously untreated patients, should provide some comparative information.
Susan O’Brien, MD
|
|
“In general, there is rarely a role for consolidation therapy to increase the depth of response in CLL.”
When I use ibrutinib, I do not believe that adding an antibody provides much additional benefit. Although you get a much faster response when an antibody is added to ibrutinib because the single agent–related lymphocytosis is abrogated, there is no benefit with respect to progression-free survival (PFS). Thus, if you are concerned about the white blood cell count, you could potentially add an antibody, but most clinicians are not too concerned about that. I generally use venetoclax in combination with rituximab, but for those who use single-agent venetoclax, you could make a case for adding rituximab if you get a lackluster response up front. In general, there is rarely a role for consolidation therapy to increase the depth of response in CLL. With lenalidomide, there are some patients who experience an improved response with a delay in disease progression and prolonged PFS. However, since lenalidomide is as myelosuppressive as chemotherapy from a neutrophil point of view, it is not an attractive strategy to add a myelosuppressive maintenance therapy to myelosuppressive chemotherapy. It is important to point out that lenalidomide is not being pursued in CLL, so it will never be indicated for CLL.
Bruce D. Cheson, MD, FACP, FAAAS, FASCO
|
|
“We have enough problems with CIT with regard to myelosuppression and infections, and to compound that with persistent immunosuppression from a monoclonal antibody or lenalidomide as maintenance therapy (without any demonstrated survival benefit) does not make sense.”
If what you mean by maintenance therapy is treatment for an extended period, then ibrutinib, by definition, is a maintenance therapy. In the context of CIT, if we are giving something such as bendamustine-rituximab, we will have a conversation with patients regarding the use of time-limited vs indefinite therapy. For the substantial proportion of those who select time-limited bendamustine-rituximab, the question is whether you want to add on another couple of years of maintenance therapy. In many contexts such as this, I am not a fan of maintenance therapy. We have enough problems with CIT with regard to myelosuppression and infections, and to compound that with persistent immunosuppression from a monoclonal antibody or lenalidomide as maintenance therapy (without any demonstrated survival benefit) does not make sense. Thus, until we have something that prolongs PFS in the absence of additional toxicity, I would not support the use of maintenance therapy. I would be careful about overinterpreting the results of the myriad of unrandomized doublet and triplet studies out there until we have more data indicating that the combinations are better than the single agents.
References
Collett L, Howard DR, Munir T, et al. Assessment of ibrutinib plus rituximab in front-line CLL (FLAIR trial): study protocol for a phase III randomised controlled trial. Trials. 2017;18(1):387.
Dartigeas C, Van Den Neste E, Léger J, et al. Rituximab maintenance versus observation following abbreviated induction with chemoimmunotherapy in elderly patients with previously untreated chronic lymphocytic leukaemia (CLL 2007 SA): an open-label, randomized phase 3 study. Lancet Haematol. 2018;5(2):e82-e94.
Flinn IW, Gribben JG, Dyer MJS, et al. Phase 1b study of venetoclax-obinutuzumab in previously untreated and relapsed/refractory chronic lymphocytic leukemia. Blood. 2019 Mar 12. pii: blood-2019-01-896290. doi: 10.1182/blood-2019-01-896290. [Epub ahead of print]
Greil R, Obrtlíková P, Smolej L, et al. Rituximab maintenance versus observation alone in patients with chronic lymphocytic leukemia who respond to first-line or second-line rituximab-containing chemoimmunotherapy: final results of the AGMT CLL-8a Mabtenance randomized trial. Lancet Haematol. 2016 l;3(7):e317-e329.
Kamisoglu K, Phipps A, Jamois C, et al. Greater efficacy of obinutuzumab compared with rituximab in chronic lymphocytic leukemia patients confirmed by a semi-mechanistic pharmacokinetic/pharmacodynamic model. Blood. 2017;130:1267.
Kater AP, Brown JR. Ibrutinib: searching for a partner drug. Lancet Oncol. 2019;20(1):3-5.
Kater AP, Seymour JF, Hillmen P, et al. Fixed duration of venetoclax-rituximab in relapsed/refractory chronic lymphocytic leukemia eradicates minimal residual disease and prolongs survival: post-treatment follow-up of the MURANO phase III study. J Clin Oncol. 2019;37(4):269-277.
Rawstron A, Munir T, Brock K, et al. Ibrutinib and Obinutuzumab in CLL: Improved MRD response rates with substantially enhanced MRD depletion for patients with >1 year prior ibrutinib exposure. Abstract presented at: 60th American Society of Hematology Annual Meeting & Exposition; December 1-4, 2018; San Diego, CA. Abstract 181.