Oncology
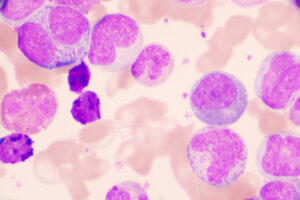
Chronic Lymphocytic Leukemia
Scientific Advancements in the Treatment of Chronic Lymphocytic Leukemia
Overview
Our featured experts have seen a remarkable transformation in the treatment of chronic lymphocytic leukemia (CLL) in the span of their careers. Advancements have allowed for a more patient-friendly treatment paradigm.
What are some of the biggest scientific advances in CLL in recent times?
Jeff Sharman, MD
|
|
“We have gone from the brute force of chemotherapy to the nuance of targeted therapy in CLL.”
We have improved both the efficacy and the tolerability of the patient treatment experience. We have gone from the brute force of chemotherapy to the nuance of targeted therapy in CLL. This is primarily a story about Bruton tyrosine kinase (BTK) and BCL-2 inhibitors, as well as the role of improved anti-CD20 antibodies. BTK and BCL-2 inhibitors have demonstrated superiority to our traditional chemoimmunotherapy regimens, and obinutuzumab represents an improvement over rituximab for those patients with CLL.
I think that we are on the cusp of further breakthroughs in immunotherapy. There is progress with bispecific antibodies and anti-CD19–directed therapies in the form of either passive antibodies or chimeric antigen receptor T-cell therapy; engaging the immune system is a common theme across all of oncology, and there will be further developments in CLL.
Additionally, I believe that further refinements in our ability to target BTK are on the horizon—in the treatment of CLL and other malignancies. We have first-generation ibrutinib, second-generation acalabrutinib and zanubrutinib, and third-generation pirtobrutinib and nemtabrutinib, which are noncovalent BTK inhibitors with improved pharmacokinetics. I think that we will see additional mechanisms for targeting BTK, whether by inhibition or by degradation, and many more changes will be forthcoming.
John C. Byrd, MD
|
|
“We have moved from non–patient-friendly therapies that mostly palliate or only modestly improve CLL outcomes to therapeutic approaches that are now much more targeted and patient friendly.”
There has been tremendous progress made over the last 20 years that I have been practicing. New treatments have come forward at different times that have transformed the patient experience. We have moved from non–patient-friendly therapies that mostly palliate or only modestly improve CLL outcomes to therapeutic approaches that are now much more targeted and patient friendly.
While treatments such as the FCR regimen (fludarabine, cyclophosphamide, and rituximab) may still be an option for consideration in very carefully selected patients, the discussions are long and complex, as risks include increased rates of secondary cancers such as myelodysplastic syndrome and acute myeloid leukemia.
In the new paradigm, even though many individuals with CLL today will require continuous treatment, virtually all patients have a good chance of surviving their disease. In fact, with the newer targeted therapies, we are at the point now where most people are living as long as they would have without the CLL.
Ian W. Flinn, MD, PhD
|
|
“To me, among the most exciting scientific advances has been the depth of the remission that we are now able to achieve with novel agent combinations.”
There has been a huge change, just in the span of my career. We have gone from the clinical trial of chlorambucil vs fludarabine by Rai et al, when we had single-digit fludarabine complete remission rates, all the way to modern nonchemotherapy-based regimens that provide minimal residual disease (MRD) rates that are well above 50%, with 75% of patients achieving undetectable MRD. Until recently, we had not been looking at MRD as an end point or a surrogate for how we treat patients.
To me, among the most exciting scientific advances has been the depth of the remission that we are now able to achieve with novel agent combinations. The responses are deeper than they were in the chemoimmunotherapy era, and there may be a subset of patients who can achieve a “functional cure” (eg, patients with a favorable prognosis who are likely to benefit from these very deep remissions), perhaps a group similar to those who were treated with FCR and their disease never came back.
While there has been a tremendous change in the way we treat patients with CLL over the last decade, many unanswered questions remain, including whether all patients should be treated the same. Although we already treat patients with 17p deletion differently, there may be other groups of patients who would benefit from a more tailored approach. For instance, those with a favorable risk profile might not require the same duration of therapy as some other patients. So, there is still much work to be done.
References
Al-Sawaf O, Gentile B, Devine J, et al. Health-related quality of life with fixed-duration venetoclax-obinutuzumab for previously untreated chronic lymphocytic leukemia: results from the randomized, phase 3 CLL14 trial. Am J Hematol. 2021;96(9):1112-1119. doi:10.1002/ajh.26260
Burger JA, O’Brien S. Evolution of CLL treatment—from chemoimmunotherapy to targeted and individualized therapy. Nat Rev Clin Oncol. 2018;15(8):510-527. doi:10.1038/s41571-018-0037-8
Egle A. Milestones in chronic lymphocytic leukemia: an exciting decade of progress—10th anniversary of Memo. Memo. 2017;10(1):8-12. doi:10.1007/s12254-017-0318-4
Rai KR, Peterson BL, Appelbaum FR, et al. Fludarabine compared with chlorambucil as primary therapy for chronic lymphocytic leukemia. N Engl J Med. 2000;343(24):1750-1757. doi:10.1056/NEJM200012143432402
Seymour JF, Gaitonde P, Emeribe U, Cai L, Mato AR. A quality-adjusted survival (Q-TWiST) analysis to assess benefit-risk of acalabrutinib versus idelalisib/bendamustine plus rituximab or ibrutinib among relapsed/refractory (R/R) chronic lymphocytic leukemia (CLL) patients [abstract 3722]. Abstract presented at: 63rd American Society of Hematology Annual Meeting and Exposition; December 11-14, 2021.
Sharman JP, Egyed M, Jurczak W, et al. Acalabrutinib with or without obinutuzumab versus chlorambucil and obinutuzmab for treatment-naive chronic lymphocytic leukaemia (ELEVATE-TN): a randomised, controlled, phase 3 trial [published correction appears in Lancet. 2020;395(10238):1694]. Lancet. 2020;395(10232):1278-1291. doi:10.1016/S0140-6736(20)30262-2
Wierda WG, Allan JN, Siddiqi T, et al. Ibrutinib plus venetoclax for first-line treatment of chronic lymphocytic leukemia: primary analysis results from the minimal residual disease cohort of the randomized phase II CAPTIVATE study. J Clin Oncol. 2021;39(34):3853-3865. doi:10.1200/JCO.21.00807