Rheumatology
Systemic Lupus Erythematosus
Cutaneous Manifestations in Systemic Lupus Erythematosus
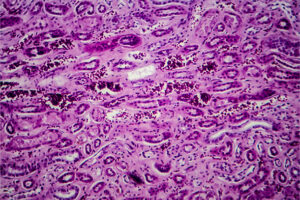
Most people who have SLE have cutaneous manifestations, and they are very often the first presenting feature of SLE. Differentiating the skin manifestations of lupus vs other skin conditions can be challenging, so you have to carefully examine patients in areas such as behind their ears, on their palms and fingers, and on their legs and trunk. You also have to examine their scalp to try to determine if there are areas where they have lost hair or areas of erythema and scaling. People get particularly upset about their hair thinning and about any kind of hair loss. This was highlighted in a poster abstract at the recent CCR East 2025 meeting discussing how much different skin symptoms bothered patients with SLE. The study reported that the most bothersome SLE-related skin symptoms were rash/redness and alopecia/hair loss. This is in line with what I see clinically.
<br>
Usually, acute cutaneous lupus erythematosus (ACLE) is identified first. A typical malar rash falls into the category of ACLE, and this type of rash appears along the nose and cheeks, classically sparing the nasolabial folds and the area right under the eyebrows. I would say that this is relatively easy to identify when you see it.
<br>
Then, with subacute CLE (SCLE), you can have lesions on the face, but they really tend to be more on the neck, trunk, body, and legs. There are 2 types of SCLE: papulosquamous and annular. The papulosquamous type can really look like psoriasis, which can make diagnosis challenging. In general, the annular plaques will often appear primarily in sun-exposed areas. I probably see that more on the top half of the body than the bottom half. People can also develop an SCLE rash after exposure to a number of medications.
<br>
Finally, we get to chronic CLE (CCLE), with the most common type being discoid. CCLE is commonly seen on the face, in the ears, and on the scalp. It can be horribly disfiguring for people because of where it appears (ie, often on the face and scalp). Discoid lupus can be a little challenging to diagnose. Early on, it can present as an erythematous plaque with a lot of scaling, and then it can spread.
<br>
In terms of prevention, the number one thing for everybody is going to be photoprotection, so we tell people to wear sunscreen all the time. I also recommend a lot of sun-protective clothing. For the treatment of cutaneous manifestations, we will often start with topical steroids and hydroxychloroquine. If those do not work, we will move on to other therapies, the choice of which depends on the severity and location of the rash, how much of the body is covered, and the medications that the patient is willing to take. If the rash is not that bad, we will use methotrexate and/or mycophenolate mofetil for CLE. In her talk at CCR East 2025, Katharina S. Shaw, MD, discussed why anifrolumab makes a lot of sense in the treatment of CLE because of the involvement of interferons in the pathophysiology of CLE. It has been shown in phase 3 trials and in clinical practice that anifrolumab is uniquely effective for cutaneous manifestations of lupus.
<br>
In addition to these agents, there are other drugs under investigation for CLE. Deucravacitinib, a TYK2 inhibitor, was previously approved by the US Food and Drug Administration (FDA) for psoriasis. In the phase 2 PAISLEY trial, which was presented in poster format at CCR East 2025, Eric F. Morand, MD, PhD, and colleagues reported that deucravacitinib met its end points for improvement in SLE. Specifically, there was improvement in the Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI-50) score (a measure of disease activity and damage in CLE) at 48 weeks in multiple patient subgroups.
Francis N, Merola J, Werth V, et al. Qualitative patient interview study in patients with systemic lupus erythematosus: patient reports of fatigue and skin-related symptoms. Poster presented at: 2025 Congress of Clinical Rheumatology East; May 1-4, 2025; Destin, FL.
<br>
Morand EF, Arriens C, Geraldino-Pardilla L, et al. Deucravacitinib in systemic lupus erythematosus: efficacy by baseline characteristics in the phase 2 PAISLEY trial. Poster presented at: 2025 Congress of Clinical Rheumatology East; May 1-4, 2025; Destin, FL.
<br>
Morand EF, Furie RA, Bruce IN, et al. Efficacy of anifrolumab across organ domains in patients with moderate-to-severe systemic lupus erythematosus: a post-hoc analysis of pooled data from the TULIP-1 and TULIP-2 trials. Lancet Rheumatol. 2022;4(4):e282-e292. doi:10.1016/S2665-9913(21)00317-9
<br>
Shaw KS. Treatment tightropes: tackling complex decisions in autoimmune skin disease. Session presented at: 2025 Congress of Clinical Rheumatology East; May 1-4, 2025; Destin, FL.
<br>
Stull C, Sprow G, Werth VP. Cutaneous involvement in systemic lupus erythematosus: a review for the rheumatologist. J Rheumatol. 2023;50(1):27-35. doi:10.3899/jrheum.220089
<br>
Xie L, Lopes Almeida Gomes L, Stone CJ, Faden DF, Werth VP. An update on clinical trials for cutaneous lupus erythematosus. J Dermatol. 2024;51(7):885-894. doi:10.1111/1346-8138.17161
<br>
This information is brought to you by Engage Health Media and is not sponsored, endorsed, or accredited by the Congress of Clinical Rheumatology.